Common Pharmacist Concerns About Generic Substitution: Perspectives from the Front Lines

When a pharmacist hands you a pill in a plain white bottle instead of the branded box you expected, it’s not just a cost-saving move-it’s a clinical decision loaded with hidden tensions. Generic substitution is one of the most powerful tools for cutting drug costs, but behind the counter, pharmacists face real, daily challenges that don’t show up in government reports. They’re caught between policy, patient distrust, physician hesitation, and the sheer weight of explaining why a $4 pill can be just as effective as a $40 one.
Why Generic Substitution Exists
The system was built to save money. Since the 1984 Hatch-Waxman Act, the FDA has allowed generic drugs to enter the market after proving they’re bioequivalent to brand-name versions. That means the active ingredient is identical, and the body absorbs it within 80% to 125% of the original. On average, studies show a 3.5% difference in absorption between brand and generic versions-statistically insignificant for most patients. The result? Generics cost about 21% less on average, and they make up over 90% of prescriptions filled in the U.S. today. But here’s the catch: just because a drug is approved doesn’t mean patients, doctors, or even pharmacists fully trust it. The gap between science and perception is wide, and pharmacists are the ones who have to bridge it-often in under three minutes.Patient Resistance: More Than Just Price
Most pharmacists will tell you the biggest hurdle isn’t policy or paperwork-it’s patient fear. Patients don’t always understand that a generic isn’t a cheaper version of the same drug. They think it’s a different drug. A 2015 survey found that 64% of patients had never heard from their doctor that a generic was an option. So when they pick up their prescription and see a different color, shape, or label, panic sets in. One woman in Austin told her pharmacist she refused the generic because it "looked like something from a discount store." Another man with high blood pressure insisted his brand-name pill "worked better"-even though his blood pressure numbers hadn’t changed in six months. The problem is worse for chronic conditions. While 82% of patients accept generics for short-term issues like infections, only 72% accept them for long-term conditions like diabetes or epilepsy. Why? Because they’re scared. They’ve heard stories. They’ve seen packaging changes. They don’t trust foreign manufacturers. And frankly, they’ve been left in the dark. Pharmacists often spend extra time walking patients through the FDA’s bioequivalence standards. Some use a simple analogy: "Think of it like two identical cars-one made in Michigan, one in Ohio. Same engine, same fuel efficiency. Just different factory." But not everyone buys it.Clinical Gray Zones: When Substitution Gets Risky
Not all drugs are created equal. Pharmacists worry most about drugs with a narrow therapeutic index (NTI)-medications where even a tiny change in blood levels can cause harm. Examples include warfarin, levothyroxine, phenytoin, and lithium. For these, the 3.5% average absorption difference doesn’t feel so small. One pharmacist in Ohio reported a patient who switched from a brand-name anti-seizure drug to a generic and had a seizure within two weeks. The patient wasn’t non-adherent. The dose was correct. But the slight difference in absorption-combined with the patient’s sensitivity-was enough to tip the balance. The case made national headlines. The FDA says generics are safe. But pharmacists know: science doesn’t always match lived experience. That’s why many pharmacists avoid substituting NTI drugs unless the prescriber explicitly allows it. Some states even require written consent before substituting these drugs. In Texas, pharmacists must document every substitution for levothyroxine. In California, they can’t substitute without checking the prescriber’s notes. Biosimilars add another layer. These are complex biologic drugs-like insulin or rheumatoid arthritis treatments-that aren’t exact copies of the original. They’re similar, but not identical. The FDA requires extra testing, and pharmacists have to be extra careful. Many pharmacists say they’re still waiting for clearer guidelines before routinely substituting them.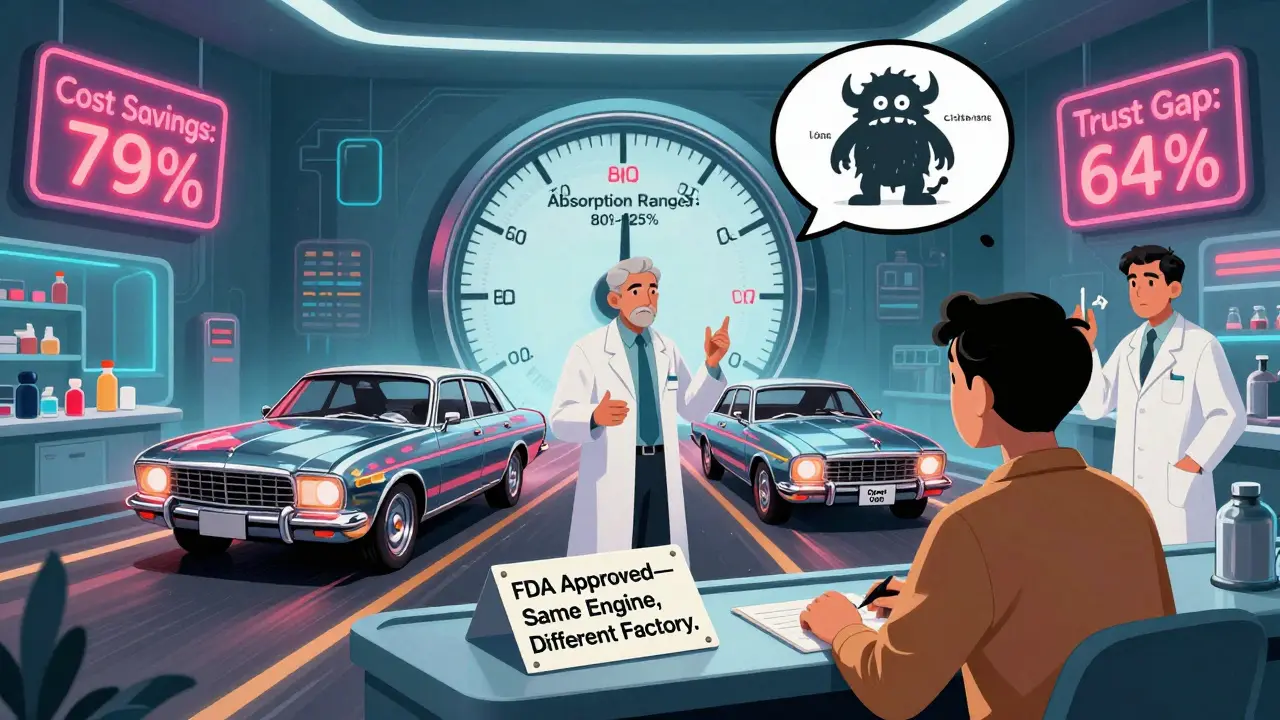
The Education Burden: Who’s Responsible?
Here’s the uncomfortable truth: pharmacists are the ones left explaining a system no one else talks about. A 2015 study found that while 79% of patients were told substitution was possible, only 38% were told they could refuse it. Only 52% were told about the price difference. That means most people walk into the pharmacy thinking they’re being forced into a cheaper option-not offered a choice. Pharmacists don’t have time to give 10-minute lectures. But they still have to answer questions like: "Why is this one blue and the last one was yellow?" or "Is this made in China?" or "Will it work as well?" Some pharmacists carry laminated cards with simple graphics showing FDA equivalence standards. Others use the phrase: "The FDA requires generics to work the same way, in the same amount of time, as the brand. If it didn’t, it wouldn’t be approved." But the real solution? Doctors need to talk about this before the patient even gets to the pharmacy. When a physician says, "I’m switching you to a generic because it’s just as effective and will save you money," patient acceptance jumps by 40%. Yet 55% of patients say they never discussed cost with their doctor.The System Is Broken-But Pharmacists Are Still Making It Work
Despite all this, pharmacists recommend generics for 96% of eligible prescriptions. They know the science. They’ve seen the data. They’ve watched patients save hundreds of dollars a year. But they’re tired. Tired of being the middleman between a broken system and confused patients. Tired of being blamed when a patient thinks their generic "didn’t work." Tired of having to educate not just patients-but also doctors who don’t understand the difference between bioequivalence and clinical equivalence. In urban pharmacies, substitution flows smoothly. In rural areas, it’s harder. Patients travel farther. They see fewer specialists. They’re more likely to distrust unfamiliar brands. And pharmacists there often have fewer resources to explain it all.
What Needs to Change
The fix isn’t complicated:- Doctors need to initiate the conversation. Not the pharmacist.
- Patients need to be told they can refuse substitution-and how to do it.
- Pharmacists need better tools: quick-reference guides, patient handouts, and time to explain.
- States need consistent rules for NTI drugs and biosimilars.
What Patients Should Know
If you’re handed a generic:- You have the right to refuse it.
- You have the right to ask why it’s different.
- You have the right to ask your doctor if substitution is safe for your condition.
Can pharmacists substitute any generic drug without asking?
No. State laws vary, but most require pharmacists to follow specific rules. For example, substitutions for drugs with a narrow therapeutic index (like warfarin or levothyroxine) often require prescriber approval. Some states also require patient consent or documentation. Pharmacists can’t substitute if the prescription says "Do Not Substitute" or "Dispense as Written."
Are generic drugs really as good as brand-name drugs?
Yes-for the vast majority of medications. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also prove bioequivalence, meaning they deliver the same amount of drug into the bloodstream within a very tight range (80-125%). Studies show no meaningful difference in effectiveness for over 90% of generic drugs. However, for a small number of drugs with a narrow therapeutic index, even small differences can matter, and some patients may respond differently.
Why do generic pills look different from brand-name ones?
By law, generics can’t look exactly like the brand-name version because of trademark rules. So they’re made with different colors, shapes, or markings. These differences are purely cosmetic and don’t affect how the drug works. But patients often mistake these changes for a different medication, which can lead to confusion or refusal to take it.
Can I ask my pharmacist to give me the brand-name drug instead?
Yes. You have the right to refuse a generic substitution and ask for the brand-name drug. However, your insurance may require you to pay the full price difference. Some pharmacists will help you find a cheaper brand option or suggest patient assistance programs if cost is a concern.
Why do some doctors seem hesitant about generic substitution?
Some doctors worry about drugs with a narrow therapeutic index, where even small changes in blood levels could cause harm. Others have seen patients experience issues after switching, even if the science says it should be fine. And some are simply unfamiliar with how the generic approval process works. Education and clear communication between prescribers and pharmacists can help reduce this hesitation.
