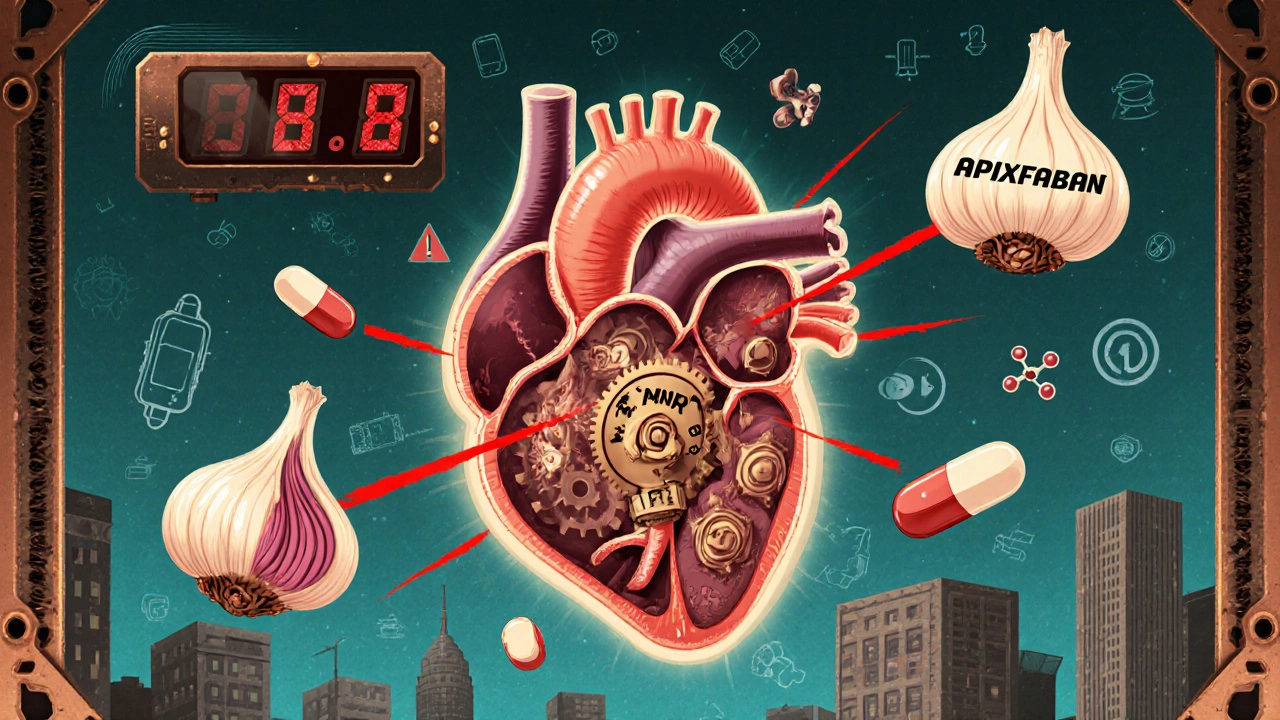
Garlic Supplements and Anticoagulants: What You Need to Know About Bleeding Risk
Blood Thinner & Garlic Risk Calculator
Assess Your Risk
This calculator determines your risk of bleeding when taking garlic supplements with anticoagulant medications based on medical research.
Many people take garlic supplements thinking they’re just helping their heart or boosting immunity. But if you’re on a blood thinner like warfarin, apixaban, or rivaroxaban, that daily pill could be putting you at serious risk. Garlic doesn’t just add flavor to your food-it can interfere with how your blood clots, and when mixed with anticoagulants, the result can be dangerous, even life-threatening bleeding.
How Garlic Affects Your Blood
Garlic contains a compound called ajoene, which stops platelets from sticking together. Platelets are the tiny cells in your blood that form clots to stop bleeding. When they can’t clump, your blood thins. This sounds good if you’re trying to prevent clots-but it’s a problem when you’re already taking medicine to do the same thing.
Studies show that standard garlic supplements (600-1,200 mg of dried powder daily) can reduce platelet function by 20-40%. That’s similar to low-dose aspirin. But unlike aspirin, which wears off in a day or two, garlic’s effect lasts up to 72 hours. And because it blocks platelets irreversibly, your body has to make new ones-taking 7 to 10 days to recover fully. That’s why even stopping garlic a few days before surgery isn’t always enough.
Why This Matters With Blood Thinners
Anticoagulants work differently than garlic. Warfarin slows down clotting factors in your liver. DOACs like apixaban block specific proteins that help clots form. Garlic doesn’t directly affect these proteins-but it adds another layer of thinning on top. The combination doesn’t just add up; it multiplies the risk.
Case reports show real harm. One man on apixaban started taking 900 mg of garlic daily and ended up in the ER with nosebleeds that wouldn’t stop for 30 minutes. Another, older patient developed a spinal hematoma from a garlic dose of 2,400 mg per day-no injury, no fall, just supplements and medication. In surgery, doctors have seen uncontrolled oozing from incisions in patients who didn’t even think garlic counted as a supplement.
For people on warfarin, garlic can push INR levels up by 1.0 to 2.5 points. Normal therapeutic range is 2.0-3.0. Go above 4.0, and spontaneous bleeding becomes likely. That’s not theoretical-it’s documented in multiple clinical studies.
Not All Garlic Is the Same
Here’s where things get tricky: garlic supplements vary wildly in strength. Aged garlic extract, like Kyolic, has almost no ajoene and is much safer. Powdered garlic pills? They can contain 0.1-0.3 mg of ajoene per gram. Garlic oil? Up to 1.0 mg per gram-the strongest form.
Most people don’t know this. Labels rarely say how much ajoene is in each pill. The FDA warned in 2021 that potency can differ by up to 15 times between brands. A supplement labeled “1,000 mg garlic” could be harmless-or it could be as potent as a full clove of raw garlic. And since most people don’t realize garlic is a supplement, they don’t mention it to their doctor.
Who’s at Highest Risk?
You’re at greater risk if you:
- Take warfarin, apixaban, rivaroxaban, dabigatran, or edoxaban
- Are over 65 (18.3% of older adults take garlic supplements)
- Are scheduled for surgery, dental work, or any procedure that involves cutting
- Have a history of bleeding, ulcers, or low platelet count
- Take other supplements like ginkgo, fish oil, or ginger
Over 3.1 million Americans over 65 are on anticoagulants and also taking garlic supplements. Most don’t know they’re combining two blood-thinning agents. A 2022 survey found 83% of garlic users had no idea it could interact with blood thinners. And 67% never told their doctor about it.
What the Experts Say
The American Society of Anesthesiologists classifies garlic as a high-risk herbal product. Their 2022 guidelines say to stop it 14 days before any surgery. The European Society of Anaesthesiology says 7 days-but even that’s not always enough, given how long garlic’s effects last.
Dr. Pieter Cohen from Harvard says garlic can increase the effects of blood thinners, leading to bleeding. The American Heart Association warns that garlic supplements should be used with extreme caution in anyone on anticoagulants. The European Medicines Agency now requires garlic supplements to carry contraindications for people on blood thinners.
Some studies downplay the risk. A 2018 meta-analysis found only small INR increases. But those studies didn’t account for high-dose garlic oil or long-term use. Real-world cases-like the two colorectal surgery patients who bled uncontrollably and needed emergency ileostomies-prove the danger isn’t just theoretical.

What You Should Do
If you’re on a blood thinner:
- Stop all garlic supplements-pills, oils, extracts-at least 14 days before any surgery or dental procedure.
- Don’t assume “natural” means safe. Garlic is a drug interaction waiting to happen.
- Ask your doctor or pharmacist: “Is garlic safe with my medication?” Don’t wait for them to ask you.
- Read supplement labels carefully. Look for “ajoene-free” or “aged garlic extract.” Avoid garlic oil or raw garlic powder.
- If you’ve been taking garlic and notice unusual bruising, nosebleeds, or blood in urine or stool, stop immediately and contact your provider.
Even if you feel fine, don’t wait for symptoms. Bleeding from this interaction can be silent at first-then sudden and severe.
The Bigger Picture
The garlic supplement market is booming. Sales hit $1.27 billion in 2022, with 28% annual growth in the U.S. But regulation hasn’t kept up. Only 42% of brands follow FDA labeling standards. Only 37% link to official interaction databases like LiverTox.
Some companies are responding. Kyolic now markets “ajoene-free” aged garlic, claiming 98% less antiplatelet activity. But without independent testing, those claims are hard to verify.
The NIH is funding a $2.4 million study to measure exactly how garlic affects DOACs like apixaban. Results are expected by late 2024. Until then, caution is the only reliable guide.
Bottom Line
Garlic supplements aren’t harmless. If you’re on a blood thinner, they’re a hidden danger. The benefits-modest blood pressure drops, cholesterol improvements-are small compared to the risk of internal bleeding, emergency surgery, or death. There’s no safe dose when you’re on anticoagulants. The only proven strategy is to stop them completely.
Don’t rely on labels. Don’t assume your doctor knows. And don’t wait for a problem to happen. Talk to your provider now. Your blood-and your body-will thank you.
Can I still eat garlic if I’m on blood thinners?
Yes, eating normal amounts of fresh or cooked garlic in food is generally safe. The risk comes from concentrated supplements-pills, oils, extracts-that deliver far more active compounds than you’d get from food. A clove or two in your pasta won’t cause issues. But taking 1,000 mg of garlic powder daily? That’s a different story.
How long should I stop garlic before surgery?
Most guidelines recommend stopping garlic supplements at least 14 days before surgery. This gives your body time to replace all the inhibited platelets. Some European guidelines say 7 days, but because garlic’s effect lasts up to 72 hours and platelet recovery takes 7-10 days, 14 days is the safer choice, especially for major procedures like heart, brain, or spine surgery.
Are there garlic supplements that are safe with blood thinners?
Aged garlic extract (like Kyolic) has very low levels of ajoene and appears to have minimal antiplatelet effects. Some manufacturers now label their products as “ajoene-free.” But since labeling isn’t standardized, you can’t always trust it. If you’re unsure, avoid all garlic supplements unless your doctor confirms a specific brand is safe.
Can garlic supplements affect my INR test results?
Yes. Studies show garlic can raise INR levels by 1.0 to 2.5 points in people taking warfarin. That could push you from a safe range (2.0-3.0) into a dangerous zone (above 4.0), where spontaneous bleeding becomes likely. If you’re on warfarin and taking garlic, your INR may become unpredictable, requiring more frequent testing-or worse, leading to emergency treatment.
What should I tell my doctor about my supplements?
Be specific. Don’t just say “I take herbs.” Say: “I take garlic pills every day,” or “I use garlic oil drops.” Mention the brand, dosage, and how long you’ve been taking it. Many patients don’t think of garlic as a supplement, so your doctor won’t ask unless you bring it up. Write it down before your appointment to make sure you don’t forget.
Are there safer alternatives to garlic for heart health?
Yes. For blood pressure and cholesterol, focus on proven lifestyle changes: regular exercise, reducing sodium, eating more fiber, and using olive oil. If you need something supplemental, omega-3s from fish oil (at low doses, 1 g/day) are a safer option than garlic, with less bleeding risk. Always check with your doctor first-even “safe” supplements can interact.

Destiny Annamaria
November 19, 2025 AT 12:07I took garlic pills for months thinking they were just 'natural heart helpers'... then I started bruising like a grape. My doc nearly had a heart attack when I told him. Turns out I was on apixaban and didn't even realize garlic was a supplement. Now I'm all about aged garlic extract and I tell everyone. Don't be me. Talk to your doctor before popping anything that smells like a kitchen.
Also, why do we treat supplements like they're candy? 🤦♀️
Nosipho Mbambo
November 19, 2025 AT 22:30Okay, but… is this really a thing? I mean, garlic is just… garlic. People have been eating it for centuries. Now we’re acting like it’s a controlled substance? 😴
Katie Magnus
November 20, 2025 AT 15:59Oh my god. I just threw out my entire bottle of garlic oil. Like, I thought it was ‘immune boosting magic’-turns out it’s just liquid bleeding risk?? I feel like a fool. Also, why does the FDA let this stuff be sold without warning labels?? I’m calling my senator.
Also, I’m now convinced every supplement company is just a cult that sells snake oil with a fancy logo. 🙃
King Over
November 22, 2025 AT 00:28Garlic supplements are dumb. Eat the real stuff. Don't take pills. Done.
Also, stop worrying so much.
Johannah Lavin
November 22, 2025 AT 10:18Y’all. I’m a 72-year-old grandma who takes warfarin and eats garlic bread every Sunday. My doctor said it’s fine because it’s FOOD. But when I started taking those ‘heart health’ capsules? Ohhhhh no. I got a nosebleed during yoga. Not fun. 😅
So if you’re on blood thinners-stick to the garlic in your pasta. Skip the pills. Your body will thank you. And if you’re not sure? Ask your pharmacist. They’re the real MVPs. 💕
Ravinder Singh
November 23, 2025 AT 12:13As someone who’s been on rivaroxaban for 5 years and used to crush 3 garlic cloves daily with honey-let me tell you, the difference between food and supplement is NIGHT and DAY.
Food = gentle, slow, harmless. Supplement = chemical grenade in a capsule.
I switched to aged garlic extract after reading this, and my INR has been stable for 8 months. Also, I now tell every Indian aunty I know who takes ‘natural blood thinners’ to stop. They think I’m crazy. But I’ve seen the ER reports. It’s not worth it.
And yes, I know you think ginger and turmeric are ‘safe’-they’re not. Same game, different spice. 🙏
Russ Bergeman
November 23, 2025 AT 13:56So… you’re telling me I can’t take garlic pills? But I read on Reddit that they lower cholesterol? And my cousin’s friend’s dentist said they’re ‘good for gums’? So… what’s the real story? Are you just trying to sell more warfarin? 🤔
Dana Oralkhan
November 24, 2025 AT 19:43My mom is 81 and takes garlic supplements because she’s ‘trying to prevent dementia.’ She’s also on Eliquis. She didn’t know it was risky until I found this article and printed it out. She cried. Then she threw out the bottle.
Thank you for writing this. So many people don’t realize supplements aren’t regulated like drugs. We need more awareness. I’m sharing this with my book club. 💛
Jeremy Samuel
November 26, 2025 AT 05:39Garlic? Pfft. I’ve been taking 3000mg a day for 10 years. No bleeding. No issues. Maybe you just need to chill. Also, the FDA is full of crap. 😎
Ron and Gill Day
November 27, 2025 AT 22:17This is why Americans are so paranoid. You think a clove of garlic is going to kill you? You’re on blood thinners? Maybe you should stop taking them. Or at least stop being so weak. This article is fearmongering dressed up as science. I’ve seen people die from being too scared to take anything. Pathetic.
Matthew Peters
November 28, 2025 AT 14:33Wait-so if I eat a whole head of roasted garlic every night, I’m fine? But if I take 1000mg of powdered garlic? That’s dangerous? That’s wild. So it’s not the garlic-it’s the concentration? That’s actually kinda cool. I never thought about it like that. I’m gonna ask my pharmacist about aged garlic extract. Thanks for this.