How progesterone can help with insulin resistance and diabetes
Understanding Progesterone and its Role in our Body
Let's start by understanding what progesterone is. Progesterone is a hormone that plays a significant role in various bodily functions, including menstrual cycles, pregnancy, and embryonic development. It is one of the most important hormones in a woman's body, but it's also present in men, albeit at lower levels. Although its primary role is often associated with reproductive health, research has shown that progesterone also plays a crucial role in other areas of health, including the management of insulin and blood sugar levels.
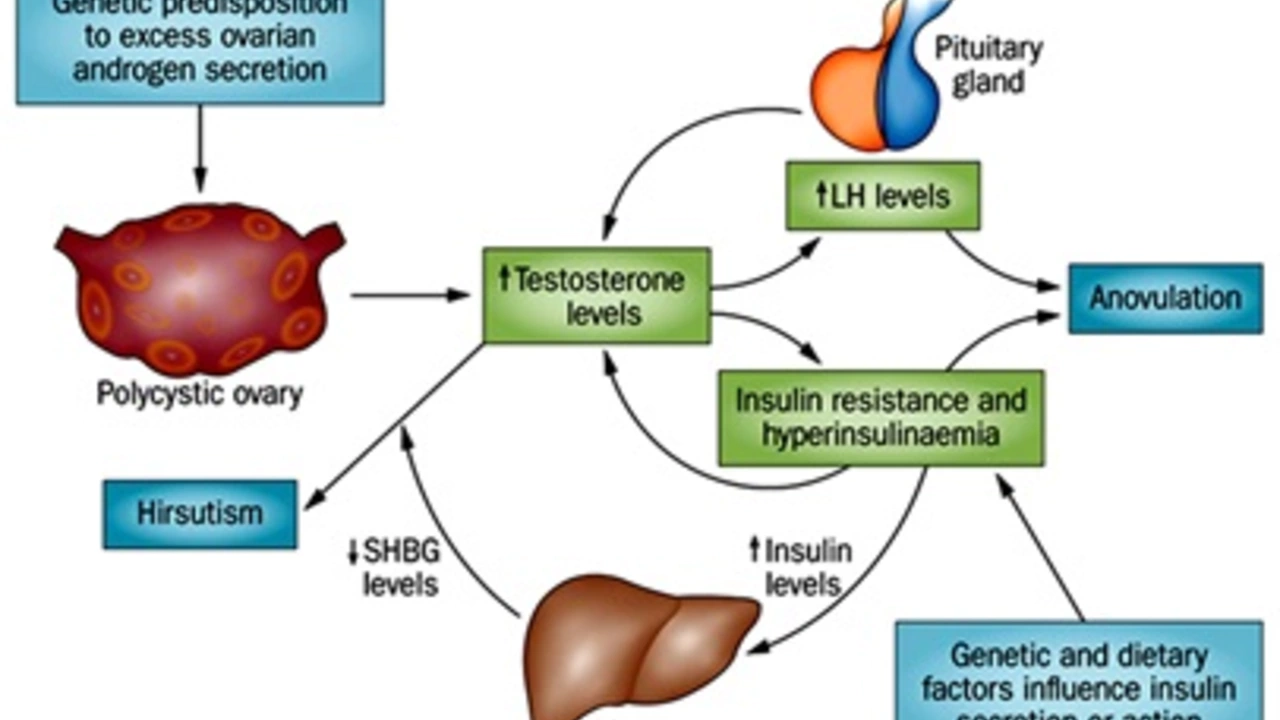
The Connection between Progesterone and Insulin Resistance
Insulin resistance is a condition where your body's cells don't respond properly to the hormone insulin. This resistance forces your pancreas to produce more insulin to keep blood sugar levels under control. Over time, this can lead to type 2 diabetes. Emerging research suggests that progesterone may help manage insulin resistance. Progesterone receptors are found in the pancreas, which secretes insulin. Studies have shown that progesterone can enhance insulin secretion and improve insulin sensitivity, reducing the risk of developing insulin resistance and diabetes.
Progesterone's Role in Diabetes Prevention
Diabetes is a chronic disease that occurs when your blood sugar levels are too high. It's a serious condition that can lead to heart disease, stroke, kidney disease, and other health problems if not managed well. Progesterone can play a vital role in preventing diabetes. Its impact on insulin production and sensitivity can help maintain a healthy blood sugar balance. By enhancing the body's response to insulin, progesterone can help prevent the onset of diabetes, especially in those who are at a high risk of developing the condition.
How to Increase Progesterone Levels Naturally
Having understood the significant role progesterone plays in managing insulin resistance and preventing diabetes, the question now becomes, how can we increase our progesterone levels naturally? There are several ways to boost progesterone levels in the body. These include maintaining a healthy weight, reducing stress, getting enough sleep, eating a balanced diet, and exercising regularly. Certain foods, such as beans, broccoli, kale, nuts, and lean meats, are also known to boost progesterone levels. However, it's important to consult with a healthcare provider before making any significant changes to your diet or lifestyle.
Progesterone Therapy: A Potential Solution for Insulin Resistance and Diabetes
For those who are unable to increase progesterone levels naturally, progesterone therapy may be a viable option. Progesterone therapy involves taking bioidentical progesterone to balance hormone levels and improve overall health. It's essential to note that this therapy should only be administered under the supervision of a qualified healthcare provider. It has been suggested that progesterone therapy can help manage insulin resistance and diabetes. However, further research is needed to fully understand the potential benefits and risks associated with this form of treatment.

Jimmy the Exploder
June 27, 2023 AT 23:28Looks like another hype piece about hormones.
Robert Jackson
June 28, 2023 AT 01:53The author exhibits a fundamental misunderstanding of endocrinology, conflating correlation with causation, and neglects the rigorous pharmacokinetic data that unequivocally demonstrate the limited efficacy of exogenous progesterone in glycemic regulation. Such oversimplifications are not only scientifically untenable but also potentially hazardous to patients.
Robert Hunter
June 28, 2023 AT 04:06In many cultures hormone balance is approached holistically, integrating diet, stress management, and community support, so the idea of a single hormone fixing insulin resistance feels overly reductionist. Nonetheless, the premise invites valuable cross‑cultural dialogue about integrative health practices.
Shruti Agrawal
June 28, 2023 AT 06:20I get why this sounds hopeful it’s nice to see natural options being discussed.
Katey Nelson
June 28, 2023 AT 08:33When we stare into the abyss of metabolic dysfunction, we are forced to confront the very essence of what it means to be a biochemical creature on this planet, and yet the humble progesterone, often relegated to the sidelines of reproductive discourse, steps forward like a quiet philosopher offering a subtle key to unlock the gates of insulin sensitivity 😏.
One could argue that the body’s endocrine symphony is a delicate dance, each hormone a dancer whose timing and grace dictate the overall performance, and progesterone, with its nuanced receptors in pancreatic tissue, may indeed cue the insulin‑producing beta‑cells to perform with greater fidelity.
However, the temptation to crown it as a panacea must be resisted, for every biochemical hero carries a shadow, and the risk of overstimulation or hormonal imbalance looms like an unwelcome guest at the feast.
Nevertheless, embracing lifestyle measures-balanced nutrition, stress reduction, adequate sleep-creates the fertile soil in which any hormonal intervention can truly flourish.
In this light, progesterone becomes less a miracle drug and more a supporting actor in a grand, multifaceted drama of health.
So, while the research is intriguing, we must temper optimism with caution, ensuring that the quest for metabolic harmony never loses sight of the broader ecological context in which our bodies reside 🌱.
Joery van Druten
June 28, 2023 AT 10:46For those considering progesterone supplementation, it’s essential to first verify serum levels through a reliable lab test. Following that, a qualified endocrinologist can help weigh potential benefits against risks such as mood changes or lipid alterations. In any case, lifestyle optimization remains the foundation of insulin sensitivity.
Melissa Luisman
June 28, 2023 AT 13:00Stop cherry‑picking studies that only support your narrative; the evidence is far from conclusive.
Akhil Khanna
June 28, 2023 AT 15:13Hey friends 😊, remember that every body is unique, so what works for one might not for another – don’t forget to listen to your own signals and seek professional guidance. Keep sharing your journeys, we all learn together! 🌟
Zac James
June 28, 2023 AT 17:26From a neutral standpoint, the article raises interesting points but more peer‑reviewed data are needed before changing clinical practice.
Arthur Verdier
June 28, 2023 AT 19:40Oh sure, because the pharma companies have been hiding the miracle of progesterone from us all along… 🙄.
Breanna Mitchell
June 28, 2023 AT 21:53Great read! Even if you’re skeptical, trying simple lifestyle tweaks alongside any hormone therapy can only help your overall wellness.
Alice Witland
June 29, 2023 AT 00:06Interesting take, though I can’t help but notice the over‑reliance on a single hormone – perhaps the author missed the forest for the trees.
Chris Wiseman
June 29, 2023 AT 02:20We stand at the crossroads of biochemistry and philosophy, where the whisper of progesterone invites us to question the very architecture of metabolic destiny. Does a single molecule truly possess the power to rewire the intricate lattice of insulin signaling, or is it but a metaphor for the larger tapestry of hormonal harmony?
The ancient sages might have argued that balance, not singularity, governs health, and modern science continues this dialogue through randomized trials and mechanistic studies.
Yet, when research uncovers progesterone receptors nestled within pancreatic beta cells, we are reminded that the body is a mosaic, each piece subtly influencing the whole.
One could posit that augmenting progesterone may tip the scales toward improved glucose uptake, but we must also contemplate the shadow side – potential dysregulation of the hypothalamic‑pituitary‑adrenal axis, mood fluctuations, and lipid perturbations.
Thus, the narrative must be tempered with caution, embracing both the promise and the perils.
In practice, clinicians should employ a holistic lens: diet, exercise, sleep, stress reduction, and, where appropriate, calibrated hormone therapy.
Only then can we hope to orchestrate a symphony where progesterone plays its modest yet meaningful part.
Remember, the pursuit of metabolic health is not a sprint but a marathon, demanding patience, perseverance, and a willingness to interrogate our assumptions.
So, while the data spark curiosity, they also remind us of the complexity inherent in endocrine regulation.
Let us celebrate the incremental gains, remain vigilant to adverse signals, and continue to ask: what other hidden actors await discovery in the grand theatre of human physiology?
alan garcia petra
June 29, 2023 AT 04:33Nice info! Even a small step toward better sleep can boost insulin sensitivity.
Allan Jovero
June 29, 2023 AT 06:46While the article is well‑intentioned, it omits crucial citations, misuses several medical terms, and fails to adhere to conventional style guidelines; a thorough editorial review is recommended.