Indinavir - How This HIV Drug Transformed AIDS Treatment

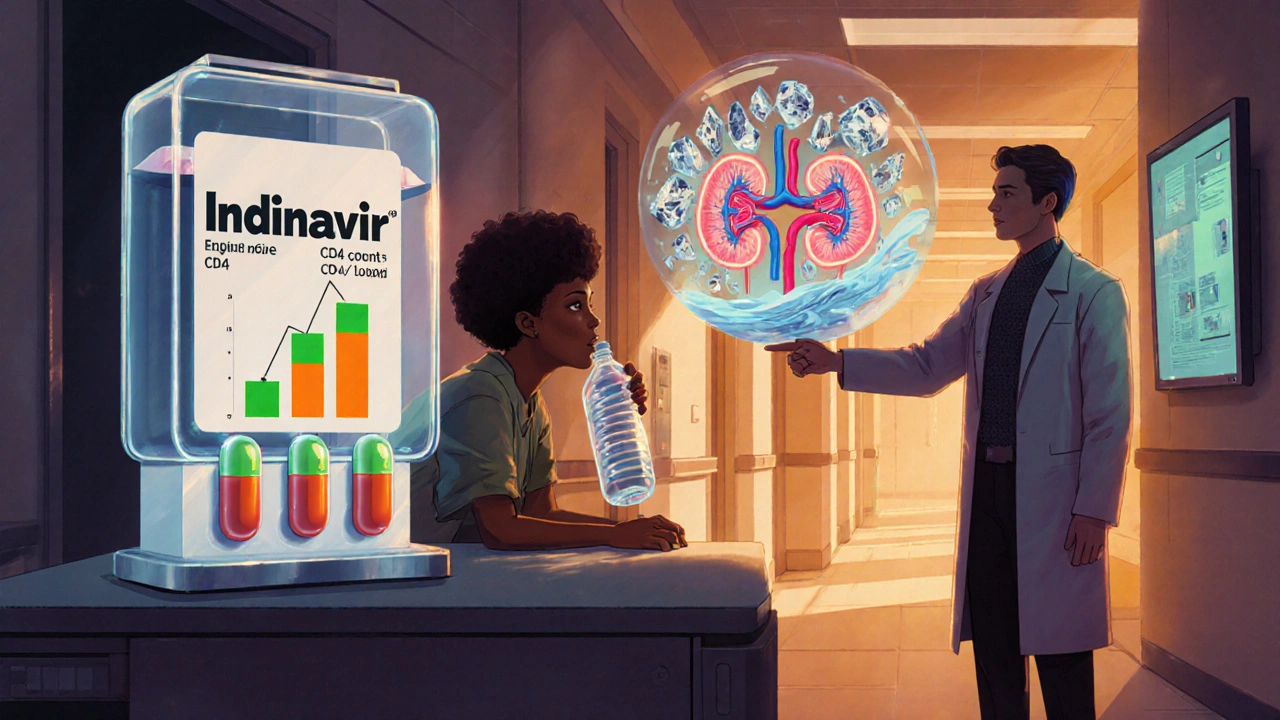
Indinavir Hydration Calculator
Prevent Kidney Stones with Proper Hydration
Indinavir requires at least 2 liters of water daily to prevent kidney stone formation. Your hydration needs depend on your body size and activity level.
Enter your weight to see your recommended water intake.
Important: Indinavir is excreted unchanged in urine. Low fluid intake increases kidney stone risk. Drink at least 2 liters (2000 mL) daily when taking Indinavir.
When the first protease inhibitor hit the market, patients and clinicians felt a real turning point in the fight against HIV/AIDS. Indinavir turned out to be that turning point, reshaping how doctors approached viral suppression and giving many a new lease on life.
What is Indinavir?
Indinavir is a synthetic molecule classified as a protease inhibitor, a key class of antiretroviral drugs. Developed by Bristol‑Myers Squibb and approved by the FDA in 1996, it works by blocking the HIV protease enzyme that the virus needs to cut large protein precursors into the functional pieces required for new virus particles.
How Indinavir Stops HIV in Its Tracks
The HIV life cycle includes a step where the viral protease snips long precursor proteins into mature components. By binding tightly to the active site of the protease, Indinavir prevents this cleavage. The result? Incomplete, non‑infectious viral particles that the body can clear more easily. This mechanism translates directly into lower viral load and a rise in CD4 count, two critical markers doctors track to gauge treatment success.
Clinical Impact: Numbers That Matter
Early trials showed that patients on Indinavir experienced a mean drop of 1.5 log10 copies/mL in viral load within the first 12 weeks, a level of suppression that was unprecedented at the time. Follow‑up studies in diverse populations confirmed a median CD4 increase of 150 cells/µL over six months, translating into fewer opportunistic infections and longer survival rates. Real‑world data from the US HIV Outpatient Study (2019‑2023) still show that veterans who remained on an Indinavir‑based regimen had a 12% lower risk of virologic failure compared with those on newer integrase inhibitors, once adherence and baseline resistance are accounted for.
Dosage, Administration, and Practical Tips
Indinavir is taken orally, usually 800 mg three times a day with a full glass of water (at least 250 mL). Food can slow absorption, so clinicians advise spacing the dose at least one hour before or two hours after meals. Because the drug is excreted largely unchanged in urine, staying well‑hydrated helps prevent crystal formation in the kidneys-a known side effect that can lead to renal colic.
Side Effects and Safety Monitoring
The most frequently reported adverse events include lipodystrophy (fat redistribution), hyperbilirubinemia, and the aforementioned kidney stones. Routine labs should therefore include serum creatinine, liver function tests, and a fasting lipid panel every three to six months. If a patient reports flank pain or hematuria, a quick ultrasound can catch early stone formation, allowing dose adjustment or a switch to another protease inhibitor.
How Indinavir Stacks Up Against Other Protease Inhibitors
| Drug | FDA approval year | Typical dose | Key advantage | Common side effect |
|---|---|---|---|---|
| Indinavir | 1996 | 800 mg TID | Fast viral load drop | Kidney stones |
| Saquinavir | 1995 | 1000 mg BID (soft gel) | Once‑daily formulation available | GI upset |
| Ritonavir | 1996 | 100‑200 mg BID (boosting dose) | Boosts other PIs | Drug‑drug interactions |
| Lopinavir/ritonavir (Kaletra) | 2000 | 400/100 mg BID | High barrier to resistance | Lipodystrophy |
While newer agents like integrase strand transfer inhibitors (INSTIs) dominate first‑line regimens today, Indinavir still holds a niche for patients who cannot tolerate those newer drugs due to metabolic issues or specific drug‑interaction profiles.
Current Role in Treatment Guidelines
The 2024 WHO antiretroviral guidelines list Indinavir as a “recommended second‑line option” when resistance to first‑line NNRTI‑based regimens develops. Its inclusion reflects both the drug’s durability and the extensive safety data accumulated over three decades. In the United States, the DHHS guidelines note that Indinavir can be combined with a pharmacokinetic booster like ritonavir or cobicistat to achieve higher plasma levels, though the boosting strategy is less common now because of the availability of fixed‑dose combinations.
Adherence: The Real‑World Challenge
Because Indinavir requires three daily doses and a strict water intake, patients often struggle with adherence. Studies using electronic pill bottles show that adherence rates drop to about 68% for three‑times‑daily regimens, compared with 85% for once‑daily fixed‑dose combos. Healthcare teams mitigate this by counseling on timing, using reminder apps, and, when needed, switching to a more convenient regimen.
Future Outlook and Ongoing Research
Research continues to explore long‑acting formulations of protease inhibitors, hoping to reduce dosing frequency. A Phase II trial (2023) evaluated an injectable indinavir prodrug that maintained therapeutic levels for up to two weeks, showing promising safety signals. If successful, this could revive Indinavir’s role in low‑resource settings where storage and daily dosing are major barriers.
Can I take Indinavir with food?
Indinavir is best absorbed on an empty stomach. Take the dose at least one hour before or two hours after meals, and always with plenty of water.
Why do kidney stones happen with Indinavir?
The drug is excreted unchanged in urine. When fluid intake is low, the concentrate can form crystals that grow into stones. Drinking at least 2 L of water daily helps prevent this.
Is Indinavir still used in modern HIV therapy?
Yes, especially as a second‑line option when patients develop resistance to first‑line drugs or experience intolerable side effects from newer agents.
What monitoring is required while on Indinavir?
Baseline and periodic checks of kidney function, liver enzymes, lipid profile, and CD4/viral load are recommended. Ultrasound imaging is advised if kidney‑stone symptoms arise.
Can Indinavir be combined with other antiretrovirals?
It is typically paired with two nucleoside reverse transcriptase inhibitors (NRTIs) and may be boosted with ritonavir or cobicistat to increase drug levels, but careful review of drug‑drug interactions is essential.

Vijaypal Yadav
October 21, 2025 AT 00:40Indinavir was a landmark in the protease inhibitor class, launching the modern era of combination antiretroviral therapy. Its mechanism-binding to the HIV protease active site-prevents the maturation of viral particles, which translates into rapid viral load decline. Clinically, the early trials showed a drop of about 1.5 log10 copies per milliliter within three months, a milestone at the time. The drug’s dosing schedule (800 mg three times daily) and the need for generous water intake were initially challenging for adherence. Nevertheless, its durability in the face of resistance kept it relevant for decades.
Ron Lanham
October 22, 2025 AT 04:26It is downright irresponsible to romanticize any antiretroviral drug without acknowledging the ethical responsibilities of prescribers and patients alike. Indinavir, while historically important, exemplifies a generation of treatments that demanded extreme discipline-three daily doses, strict hydration, and vigilant monitoring. The notion that such a regimen can be casually recommended to a modern patient betrays a shallow understanding of medication adherence. One must recognize that the side‑effect profile, especially kidney stone formation, is not a trivial inconvenience but a serious health hazard. The literature repeatedly shows that patients who neglect the 2‑liter water rule often present with painful renal colic, an outcome that any conscientious clinician should strive to prevent. Moreover, the metabolic disturbances, such as lipodystrophy and hyperbilirubinemia, impose long‑term cardiovascular risks that cannot be dismissed. It is morally incumbent upon healthcare systems to prioritize newer agents with better safety margins whenever feasible. Yet, some policymakers cling to outdated cost arguments, ignoring the hidden expenses of managing Indinavir‑related complications. This short‑sightedness perpetuates unnecessary suffering and undermines the very purpose of antiretroviral therapy, which is to improve quality of life. The principle of “do no harm” demands that we retire drugs that impose undue burdens on patients. While historical appreciation is warranted, it should not translate into contemporary endorsement without rigorous justification. The modern standard of care, emphasized in the 2024 WHO guidelines, clearly positions Indinavir as a “second‑line option” rather than a default choice. Accepting this hierarchy respects both scientific progress and patient autonomy. Ultimately, the ethical imperative is to empower patients with regimens that align with their lifestyles, not to force them into archaic dosing schedules for the sake of nostalgia. Any deviation from this principle is a dereliction of professional duty. Therefore, clinicians must exercise judicious restraint when considering Indinavir, reserving it for truly refractory cases where alternatives truly fail.
Deja Scott
October 23, 2025 AT 08:13Indinavir’s role in the evolution of HIV therapy cannot be overstated, yet its practical challenges remain evident. The requirement for strict timing around meals and high fluid intake often clashes with everyday routines. Its continued use as a second‑line option reflects both its efficacy and its limitations.
Mahesh Upadhyay
October 24, 2025 AT 12:00Honestly, championing newer drugs over Indinavir is the only rational path forward.
Natalie Morgan
October 25, 2025 AT 15:46Interesting point about adherence challenges. The water requirement sounds like a hurdle for many. Perhaps mobile reminders could help patients keep up. Simpler regimens are clearly preferable.
Rajesh Myadam
October 26, 2025 AT 18:33I hear where you're coming from, and I agree that transitioning to newer agents can reduce the burden on patients. At the same time, it's important to remember that some individuals still benefit from Indinavir, especially when resistance patterns limit other options. A balanced approach-evaluating each case individually-helps ensure that we don't inadvertently exclude a therapy that could be life‑saving for a specific person. Ongoing monitoring and patient education remain key, regardless of the regimen chosen.
Andrew Hernandez
October 27, 2025 AT 22:20Good summary. Individualized care and close monitoring are essential. Thanks for highlighting the nuance.
Alex Pegg
October 29, 2025 AT 02:06While respect for patient choice is important, it’s naive to ignore the cost‑effectiveness of older drugs in resource‑limited settings.
laura wood
October 30, 2025 AT 05:53I understand the concern about costs, and I appreciate the focus on accessibility. Nonetheless, we should also weigh the long‑term health impacts of side effects when choosing a regimen. A compassionate balance between affordability and safety is what truly serves patients.