Kyphoplasty vs Vertebroplasty: What You Need to Know About Vertebral Fracture Treatment
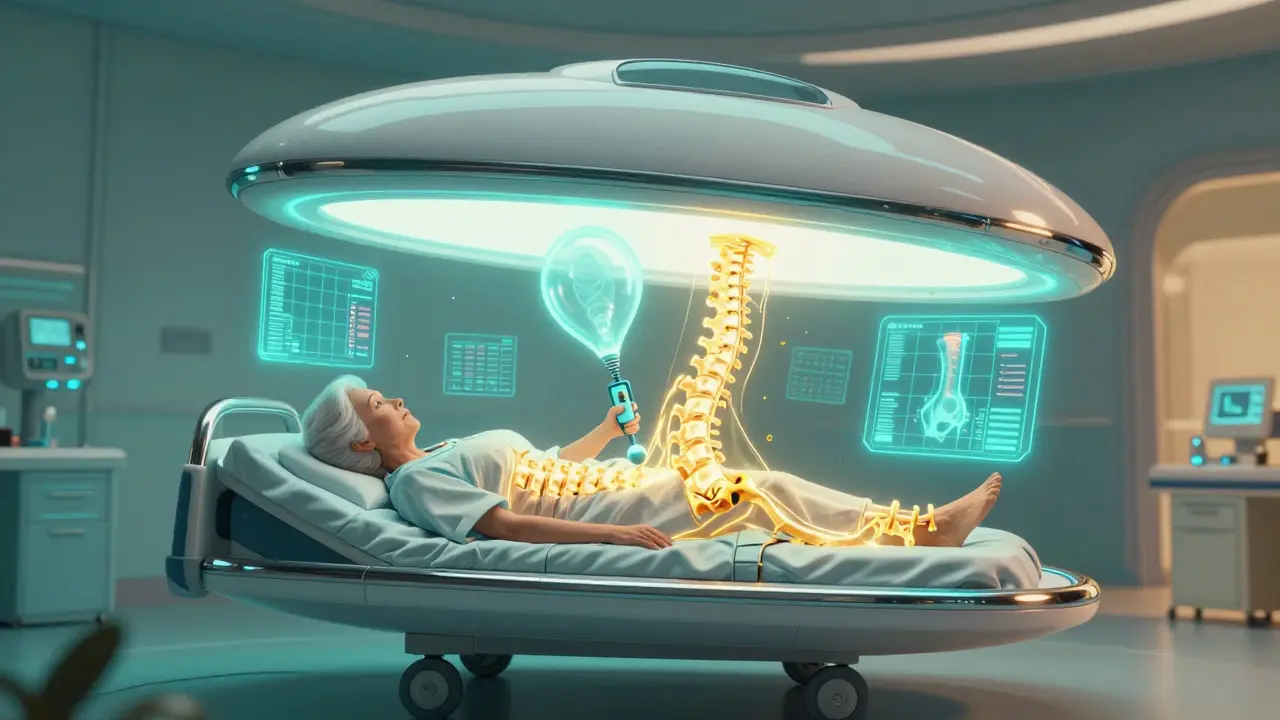
When a vertebra in your spine cracks or collapses, it’s not just a backache-it’s a life-changing event. For many older adults, especially women over 65, a simple fall or even a sneeze can lead to a vertebral compression fracture. The pain is sharp, constant, and often makes standing, walking, or sleeping impossible. For years, the only options were weeks of bed rest, painkillers, or risky open surgery. But today, two minimally invasive procedures-kyphoplasty and vertebroplasty-have changed the game. Both offer quick pain relief, same-day recovery, and a return to normal life. But which one is right for you? And does the extra cost of kyphoplasty actually make a difference?
What Happens When a Vertebra Fractures?
Vertebral compression fractures happen when the front part of a spinal bone (the vertebral body) collapses under pressure. This is most common in people with osteoporosis, where bones become thin and brittle. About 700,000 of these fractures occur in the U.S. every year. One in four women over 50 will experience one. The fracture doesn’t always show up on a regular X-ray right away. That’s why doctors rely on MRI scans to confirm it’s a fresh fracture with active inflammation-otherwise, these procedures won’t work.
Without treatment, the collapsed bone can cause a forward curve in the spine (kyphosis), leading to a hunched posture, chronic pain, and even trouble breathing. Many patients end up stuck in a cycle of pain, reduced mobility, and increased risk of more fractures. That’s where kyphoplasty and vertebroplasty come in.
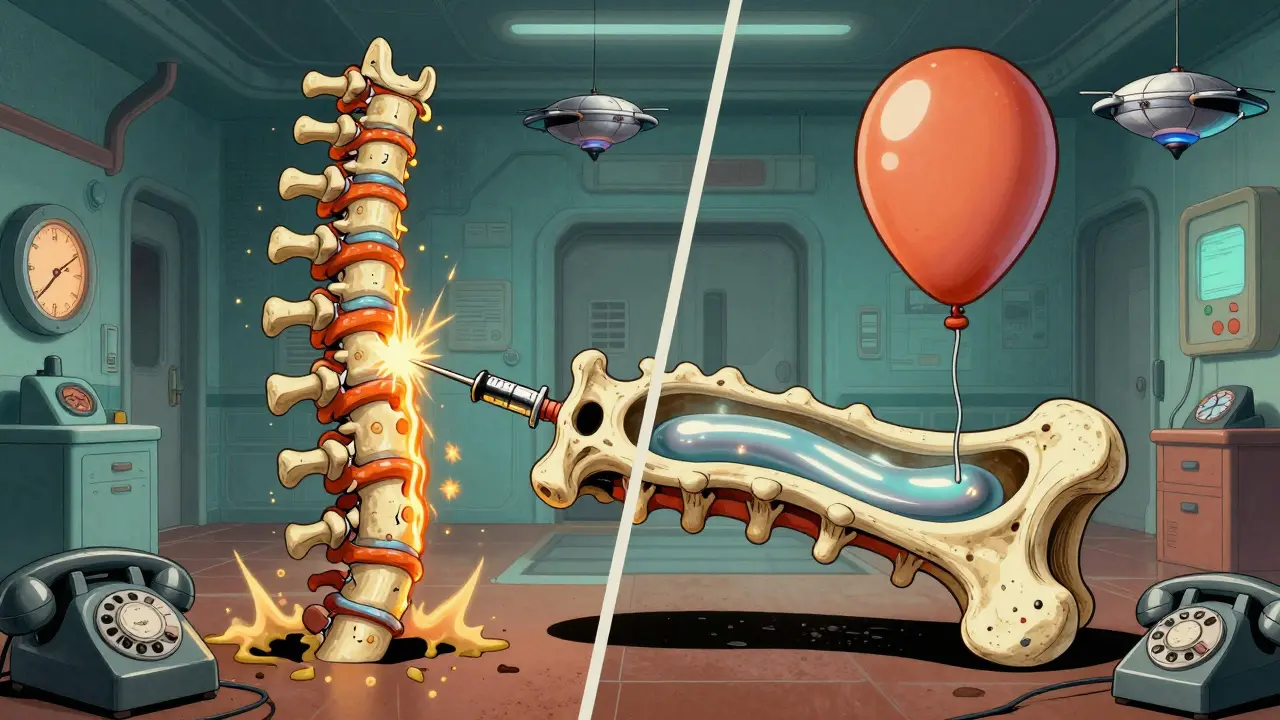
Vertebroplasty: Direct Cement Injection
Vertebroplasty is the older of the two procedures, first used in the mid-1980s. It’s straightforward: a needle is inserted through the skin into the fractured vertebra under X-ray guidance. Then, a thick, fast-hardening bone cement called polymethylmethacrylate (PMMA) is injected directly into the broken bone. The cement fills the cracks and hardens in 10 to 20 minutes, acting like an internal cast to stabilize the fracture.
The whole process takes about 30 to 60 minutes. Most patients get local anesthesia and light sedation, so they’re awake but relaxed. You’ll be on your feet the same day. Studies show 85-90% of patients report immediate pain relief, with VAS pain scores dropping from an average of 8.2 to 1.5 within 24 hours. About 75% stop using opioids within a week.
But there’s a catch. Because the cement is injected under high pressure (150-200 psi), it can leak out of the bone. Cement leakage happens in 27-68% of vertebroplasty cases. Most leaks are harmless, but in about 1.1% of cases, it can press on nerves or travel to the lungs, causing serious problems.
Kyphoplasty: The Balloon Technique
Kyphoplasty was developed in the late 1990s as an upgrade to vertebroplasty. Instead of injecting cement directly, doctors first insert a small balloon into the fractured vertebra. The balloon is inflated with saline to gently lift the collapsed bone back into place and create a hollow space inside. Once the balloon is deflated and removed, the cavity is filled with cement under lower pressure.
This extra step gives kyphoplasty two key advantages. First, it can restore some of the lost height in the vertebra-up to 40-60% in many cases. Second, because the cement is injected into a pre-formed cavity, leakage is much less common, happening in only 9-33% of cases. The risk of serious complications drops to 0.6%.
Patients report the same level of pain relief as vertebroplasty-around 85-90%. But kyphoplasty has one extra benefit: it can help straighten the spine. One Reddit user, u/OsteoWarrior87, described it as “instant relief like flipping a switch.” Another patient noted that while their vertebroplasty eased the pain, it didn’t fix their hunched back. Kyphoplasty did.
Side by Side: Kyphoplasty vs Vertebroplasty
So which is better? It depends on your fracture and your goals.
| Feature | Kyphoplasty | Vertebroplasty |
|---|---|---|
| Procedure Step | Balloon inflation first, then cement | Cement injected directly |
| Cement Pressure | Low (100-150 psi) | High (150-200 psi) |
| Cement Leakage Rate | 9-33% | 27-68% |
| Vertebral Height Restoration | 40-60% | Minimal to none |
| Typical Procedure Time | 45-75 minutes | 30-60 minutes |
| Average Medicare Cost (2023) | $3,850 | $2,950 |
| Best For | Fractures with height loss, kyphosis, unstable bones | Stable fractures without deformity |
Doctors at Mayo Clinic and Johns Hopkins agree: both procedures relieve pain equally well. But kyphoplasty’s lower leakage rate and ability to restore spine alignment make it the preferred choice for fractures with significant collapse-especially if you’re worried about posture or long-term mobility.
Who Gets These Procedures?
Not everyone with a back fracture qualifies. These procedures are only for acute fractures-those that happened within the last 6 to 8 weeks and show bone swelling on MRI. Chronic fractures, where the bone has already healed in a collapsed position, won’t respond.
Medicare and most private insurers cover both procedures if you’ve tried at least 4-6 weeks of conservative treatment: pain meds, bracing, physical therapy. About 95% of requests get approved when the paperwork is complete.
Most patients are over 65. Women make up 70-75% of cases because osteoporosis hits them harder after menopause. But men with osteoporosis or cancer-related fractures (like from breast or lung cancer that spread to the spine) are also common candidates.
What to Expect Before, During, and After
Before: You’ll get an MRI to confirm the fracture is fresh. Blood tests and a quick heart check are standard. You’ll be told to stop blood thinners a few days before. Don’t eat or drink after midnight the night before.
During: You’ll lie face down on an X-ray table. The area is numbed, and you’ll be given sedation. The doctor inserts a thin needle through your back into the fractured vertebra. For kyphoplasty, balloons are inflated and deflated. Then cement is injected. You’ll be awake but won’t feel pain.
After: You’ll rest for 4-6 hours in recovery. Most patients walk within a few hours. You’ll go home the same day. No heavy lifting or twisting for 24 hours. You can return to light activities in 2-3 days. Full recovery takes 1-2 weeks.
What Doesn’t Work
Some patients expect these procedures to fix everything. But they won’t reverse long-term damage. If you’ve had a hunched back for years, kyphoplasty can help, but it won’t make you stand completely straight. It also doesn’t cure osteoporosis. That’s why doctors always follow up with bone-strengthening meds like bisphosphonates or denosumab.
And while most people feel better right away, 10-15% still have lingering pain. Sometimes, another fracture happens nearby within a year. That’s why ongoing osteoporosis treatment is just as important as the procedure itself.
Cost, Insurance, and Value
Kyphoplasty costs about 20-30% more than vertebroplasty. Medicare pays $3,850 for kyphoplasty versus $2,950 for vertebroplasty. But here’s the thing: the higher cost doesn’t mean better pain relief. Both deliver the same results on that front.
Dr. Richard Jensen from Oregon Health & Science University found that vertebroplasty offers better value for patients without spinal deformity. For those with a visible hunch or significant height loss, kyphoplasty’s added benefit justifies the extra cost. Insurance companies are starting to notice this-some now require proof of deformity before approving kyphoplasty.
What’s New in 2026?
Recent studies are changing how we think about these procedures. The Vertos II trial, published in early 2023, showed that patients who got kyphoplasty or vertebroplasty within two weeks of their fracture had a 28% lower risk of dying within a year compared to those who only took pain meds. That’s huge. It suggests these aren’t just pain relievers-they might save lives.
Newer cement types are also emerging. Calcium phosphate cement, approved by the FDA in March 2023, is more like real bone and doesn’t generate as much heat during hardening. That could mean fewer complications down the road.
Meanwhile, the COAST trial-expected to finish in late 2024-is trying to answer whether kyphoplasty’s height restoration actually leads to better mobility and less back pain over two years. Early data suggests it might, but we’re still waiting for final results.
Final Thoughts: Which One Is Right for You?
If you have a recent fracture with severe pain and no deformity, vertebroplasty is a safe, affordable, and effective choice. If your fracture has caused your spine to curve, you’re losing height, or your bones are very weak, kyphoplasty gives you a better chance at restoring your posture and reducing long-term risks.
Both procedures are fast, safe, and life-changing for the right patient. The biggest mistake people make is waiting too long. The sooner you treat a fresh fracture, the better the outcome. Don’t wait for pain to become your new normal. Talk to your doctor about an MRI and whether one of these procedures could help you get back on your feet-quickly and safely.
Are kyphoplasty and vertebroplasty the same thing?
No. Both use bone cement to stabilize fractured vertebrae, but kyphoplasty adds a balloon step to restore height before injecting cement. Vertebroplasty injects cement directly. Kyphoplasty reduces cement leakage and can correct spinal deformity; vertebroplasty is simpler and cheaper but doesn’t restore height.
How long does pain relief last after these procedures?
Most patients feel significant pain relief within 24 hours, and the relief typically lasts for years. But the procedure doesn’t stop osteoporosis. New fractures can still happen in other vertebrae. That’s why ongoing bone-strengthening treatment is essential.
Can I go home the same day?
Yes. Both procedures are outpatient. You’ll be monitored for 4-6 hours after, then discharged. Most people walk the same day and return to light activities within 2-3 days.
Is kyphoplasty worth the extra cost?
If your fracture has caused visible spinal deformity or significant height loss, yes. Kyphoplasty’s lower risk of cement leakage and ability to restore posture make it worth the higher price. For stable fractures without deformity, vertebroplasty offers the same pain relief at a lower cost.
What are the risks of these procedures?
The main risk is cement leakage. With vertebroplasty, it happens in up to 68% of cases, though serious complications occur in only about 1.1%. Kyphoplasty reduces leakage to 9-33% and serious risks to 0.6%. Other rare risks include infection, nerve damage, or new fractures nearby. Most patients experience no major issues.
Will I need physical therapy after the procedure?
Not always, but it’s often recommended. Physical therapy helps rebuild core strength, improve posture, and prevent future falls. Your doctor may refer you to a therapist once you’re cleared to move more freely-usually after 1-2 weeks.

Candice Hartley
January 26, 2026 AT 21:02Andrew Clausen
January 28, 2026 AT 06:59Harry Henderson
January 30, 2026 AT 06:31suhail ahmed
February 1, 2026 AT 06:08Kirstin Santiago
February 1, 2026 AT 15:48Kathy McDaniel
February 2, 2026 AT 17:38April Williams
February 2, 2026 AT 19:33John O'Brien
February 3, 2026 AT 03:36astrid cook
February 4, 2026 AT 17:02Conor Flannelly
February 6, 2026 AT 06:02Marian Gilan
February 7, 2026 AT 12:53Desaundrea Morton-Pusey
February 9, 2026 AT 01:11Anjula Jyala
February 9, 2026 AT 08:53Conor Murphy
February 10, 2026 AT 03:52Murphy Game
February 11, 2026 AT 22:12