Levothyroxine and Proton Pump Inhibitors: What You Need to Know About Absorption Interactions
Levothyroxine-PPI Interaction Calculator
This tool estimates how proton pump inhibitors (PPIs) may affect your thyroid medication absorption based on clinical evidence.
Key Interaction Facts
3.2 mIU/L average TSH increase when taking PPIs with levothyroxine.
Timing doesn't matter - PPIs suppress acid for up to 72 hours.
12.5-25 mcg dose increase typically needed to maintain normal TSH.
If you’re taking levothyroxine for hypothyroidism and also use a proton pump inhibitor (PPI) like omeprazole or pantoprazole for heartburn, you might be wondering: is this combo hurting my thyroid treatment? The answer isn’t simple, but the data is clear-this interaction is real, common, and often overlooked.
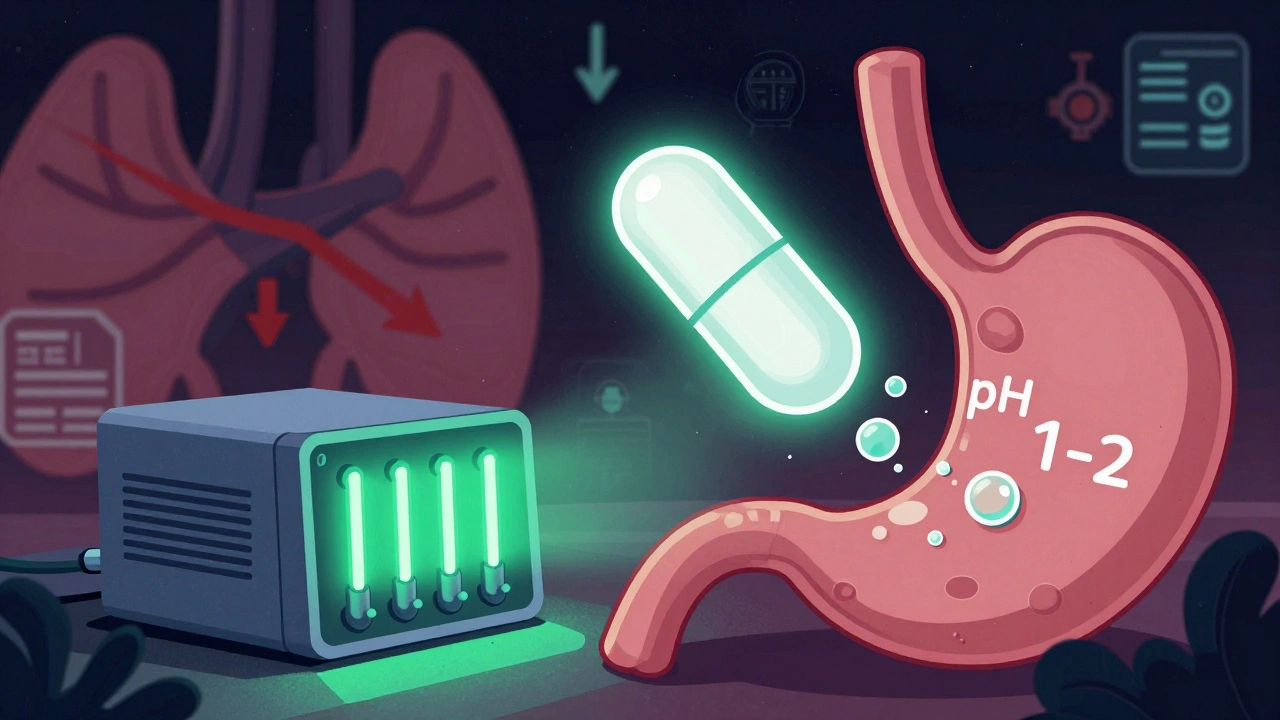
Why Levothyroxine Needs Stomach Acid
Levothyroxine isn’t like most pills. It doesn’t just dissolve in your gut and get absorbed. It needs an acidic environment to break down properly. Your stomach, normally at a pH between 1 and 2, creates the right conditions for levothyroxine to dissolve and enter your bloodstream. Without enough acid, the tablet sits there, barely absorbed. That’s why doctors tell you to take it on an empty stomach, 30 to 60 minutes before breakfast.
But when you take a PPI-medications like Prilosec, Nexium, or Protonix-that changes. These drugs shut down the acid pumps in your stomach lining. Within hours, your stomach pH rises to 4 or even 6. That’s like turning down the heat on a stove while your soup is still boiling. The levothyroxine doesn’t dissolve well. Your body absorbs less. And your thyroid-stimulating hormone (TSH) starts creeping up, even if you’re taking your pill exactly as directed.
The Evidence: It’s Not Just a Theory
A 2021 systematic review in the Journal of General Internal Medicine looked at seven studies involving over 1,200 patients. Every single one showed higher TSH levels when PPIs were taken with levothyroxine. That’s not a fluke. It’s a pattern. Even patients who were perfectly stable on their thyroid dose saw TSH rise after starting a PPI.
One 2023 study followed 40 people on levothyroxine who were given 40mg of pantoprazole daily for six weeks. Their TSH levels jumped-on average-by 3.2 mIU/L. That’s enough to trigger symptoms like fatigue, weight gain, and brain fog. And here’s the kicker: whether they took the PPI in the morning with levothyroxine or at night, the effect was the same. Separating the doses by four hours? Doesn’t help. Why? Because PPIs don’t just block acid for a few hours. They suppress it for up to 72 hours. Your stomach stays too neutral for days.
Who’s Affected?
Here’s the scale: About 20 million Americans take levothyroxine. Nearly 18% of them also take a PPI. That’s over 2.7 million people who could be under-treated without knowing it. The Mayo Clinic found that 15-20% of these patients need their levothyroxine dose increased-often by 12.5 to 25 mcg-to get TSH back into range.
And it’s not just older adults. Younger people with Hashimoto’s thyroiditis, who often have GERD or stomach issues, are increasingly caught in this trap. Reddit’s r/Hashimotos community analyzed 147 posts from late 2023. Sixty-eight percent of users reported needing higher levothyroxine doses after starting PPIs. Seventy-two percent said they felt more tired. Fifty-eight percent noticed unexplained weight gain.
What Can You Do?
There are three real options-none of them perfect, but all better than ignoring the problem.
Option 1: Increase Your Levothyroxine Dose
This is the most common fix. If you’re on a PPI and your TSH is high, your doctor may bump your levothyroxine by 12.5-25 mcg. That’s about half to one full tablet. After the change, you’ll need a blood test in 6-8 weeks to check if TSH is back in range (usually 0.5-2.5 mIU/L for most patients).
But here’s the catch: if you stop the PPI later, your dose will be too high. You could end up with hyperthyroid symptoms-racing heart, anxiety, insomnia. That’s why you need to monitor TSH regularly and adjust carefully.
Option 2: Switch to Liquid Levothyroxine
There’s a better way: Tirosint-SOL. This is a liquid form of levothyroxine that doesn’t need stomach acid to work. It’s absorbed in the upper intestine, bypassing the acidic environment entirely. A 2019 study in the Journal of Clinical Endocrinology & Metabolism confirmed it works just as well-even with PPIs.
The downside? Cost. Generic levothyroxine tablets cost $15-$25 a month. Tirosint-SOL? Around $350. Insurance might cover it if you document the interaction, but many patients can’t afford it. Still, for people who’ve struggled with absorption for years, it’s life-changing.
Option 3: Try an H2 Blocker Instead
Not all acid reducers are the same. Famotidine (Pepcid) and ranitidine (though mostly off the market now) are H2 blockers. They reduce acid too, but not as deeply or as long as PPIs. A 2018 study in Pharmacotherapy showed no significant TSH changes when famotidine was taken with levothyroxine.
If you only need mild heartburn relief, switching from omeprazole to famotidine might solve the problem without costing a fortune. But if you have severe GERD or Barrett’s esophagus, H2 blockers might not be strong enough.
What About Timing? Should I Take Them Hours Apart?
You’ve probably heard: “Take levothyroxine in the morning, PPI at night.” Sounds logical. But here’s the truth: it doesn’t work. Because PPIs don’t just turn off acid for a few hours-they suppress it for days. Even if you take your PPI at 8 p.m. and your levothyroxine at 6 a.m., your stomach is still too neutral. The 2023 pantoprazole study proved it: timing made no difference.
Dr. Elizabeth Pearce, a leading endocrinologist at Boston Medical Center, says short-term PPI use (under four weeks) rarely causes issues. But if you’ve been on one for three months or longer? You’re at risk. That’s when you need to act.

What Should You Do Right Now?
If you’re on both medications:
- Check your last TSH level. If it’s been over six months, get it tested now.
- Look at your PPI use. Are you on it daily? For more than three months?
- If your TSH is high and you’re on a PPI, don’t assume you’re just “not taking your pill right.” Talk to your doctor about this interaction.
- Ask: Can I switch to famotidine? Or try liquid levothyroxine? Or adjust my dose?
Don’t wait for symptoms to get worse. Fatigue and weight gain aren’t normal. They’re signs your thyroid isn’t getting what it needs.
What’s Next?
The FDA is working on new labeling rules for thyroid medications to highlight PPI interactions. Clinical guidelines from the American Thyroid Association are being updated in 2024 to make this a formal recommendation, not just an observation.
Meanwhile, companies are developing enteric-coated levothyroxine tablets designed to dissolve in the small intestine, not the stomach. Early trials are promising. If they get approved, this could be the game-changer for millions.
For now, the tools we have are simple: monitor, adjust, or switch. Don’t let a common heartburn pill quietly sabotage your thyroid treatment. You deserve to feel your best-and that starts with making sure your medication works the way it should.

Ada Maklagina
December 5, 2025 AT 11:05Just took my levothyroxine with coffee like always and my TSH spiked last month. Now I’m wondering if my PPI is the real culprit.
Juliet Morgan
December 5, 2025 AT 17:04i’ve been on both for 2 years and i swear i’ve gained 18 lbs and feel like a zombie. my doc said ‘maybe you’re just stressed’ lol. i switched to famotidine last week and already my energy’s coming back. no more 3pm naps. thank god.
Deborah Jacobs
December 6, 2025 AT 23:08Oh my god, this is the exact story of my life. I was convinced I was just ‘getting older’-fatigue, brain fog, weight that wouldn’t budge no matter how much I ran. Then I found a Reddit thread about PPIs and thyroid meds and cried in my oat milk latte. Switched to Tirosint-SOL after my endo finally listened. My TSH dropped from 7.8 to 1.9 in six weeks. I can now remember my kids’ birthdays again. This isn’t just medicine-it’s a lifeline.
Katie Allan
December 8, 2025 AT 05:11Thank you for writing this with such clarity. So many of us are told ‘just take it more consistently’ when the real issue is buried in pharmacology. This should be standard patient education. I’ve shared this with my thyroid support group-every single person there is either on a PPI or knows someone who is. We need better awareness, not just more pills.
Jimmy Jude
December 9, 2025 AT 09:02So let me get this straight-big pharma doesn’t want you to know that your $350 liquid thyroid pill is the only real solution because they’re making billions off omeprazole? And your doctor’s too lazy to look past the algorithm? Welcome to healthcare, folks. We’re all just lab rats with insurance cards.
Harry Nguyen
December 11, 2025 AT 00:55Of course the FDA is ‘working on labeling.’ That’s like the IRS saying they’re ‘reviewing tax loopholes.’ Meanwhile, millions are walking around tired and bloated because someone decided ‘acid suppression’ was a lifestyle upgrade. Wake up. This isn’t medicine-it’s corporate convenience dressed in white coats.
William Chin
December 11, 2025 AT 06:56As a board-certified endocrinologist with over 22 years of clinical experience, I must emphasize that the interaction between proton pump inhibitors and levothyroxine is not merely a pharmacokinetic curiosity-it is a clinically significant, evidence-based phenomenon that demands systematic intervention. The data presented in the referenced 2023 study is robust, and failure to adjust dosing accordingly constitutes a deviation from the standard of care. I urge all practitioners to implement mandatory TSH monitoring protocols for patients on chronic PPI therapy.
James Moore
December 12, 2025 AT 05:49Let’s not forget the broader philosophical implications here: we’ve outsourced our bodily autonomy to chemical buffers and corporate formularies. The stomach, once a sacred furnace of digestion and identity, is now a mere industrial valve to be switched off at will-while we numb our existential dread with oat milk lattes and 12.5 mcg thyroid tweaks. Are we healing… or just optimizing our suffering into a subscription model? Tirosint-SOL isn’t a drug-it’s a cry for meaning in a world that treats biology like a software bug.
Manish Shankar
December 13, 2025 AT 23:40As a physician practicing in Mumbai, I have observed this interaction frequently among patients with Hashimoto’s and chronic gastritis. Many are prescribed PPIs for mild symptoms without adequate evaluation. The rise in TSH levels is often dismissed as ‘non-compliance.’ I now routinely screen for PPI use in all hypothyroid patients and recommend famotidine where appropriate. This is a global issue, not just an American one.
Norene Fulwiler
December 15, 2025 AT 12:06I’m a Black woman in my 40s with hypothyroidism and GERD. My doctor kept telling me to ‘try harder’-more sleep, less sugar, more yoga. No one asked about my daily omeprazole. When I finally brought up the interaction, he looked at me like I’d spoken a foreign language. I switched to Tirosint-SOL with insurance help and now I can actually play with my kids without needing a nap. This isn’t just science-it’s justice.