Managing Hives in Pollen Season: Tips, Treatments & Prevention
Hives Emergency Assessment Tool
Emergency Assessment Tool
This tool helps determine if your hives require immediate medical attention based on symptoms. If you're experiencing any of the emergency symptoms described, seek medical help immediately.
Important Safety Information
Remember: If you experience any of the following symptoms, call emergency services immediately:
- Difficulty breathing or wheezing
- Swelling of the throat, tongue, or lips
- Severe dizziness or loss of consciousness
- Abdominal pain or vomiting with hives
For life-threatening reactions, use an epinephrine auto-injector if prescribed and call 911 immediately.
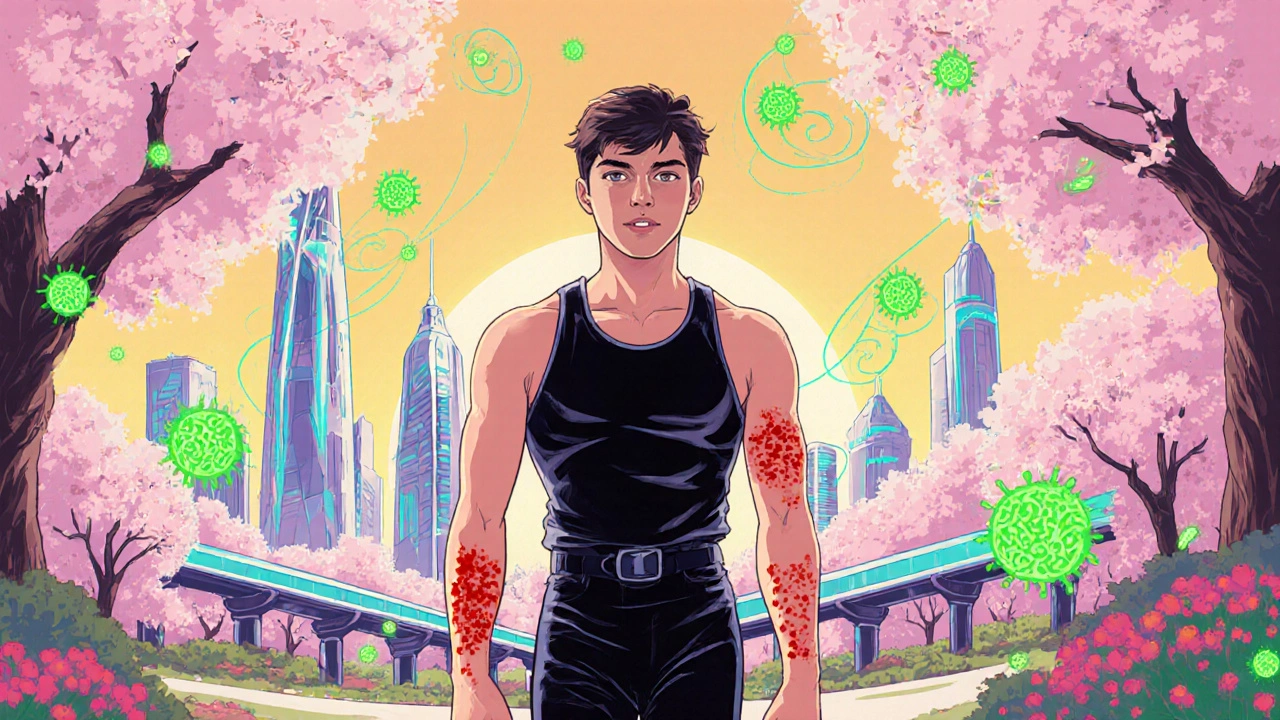
When spring rolls around, the world bursts into color and fragrance-until the pollen hits the bloodstream and your skin starts itching like crazy. Hives a skin condition also known as urticaria, marked by red, raised welts that flare up suddenly and can last anywhere from minutes to days become a frustrating side‑effect of that seasonal pollen. If you’ve ever watched the rash spread across your arms while the trees were in full bloom, you know the scramble for relief is real. This guide walks you through practical steps, from instant soothing tricks to longer‑term prevention, so you can keep the itch at bay without sacrificing the joy of spring.
Quick Takeaways
- Identify pollen as the trigger and keep exposure low with indoor air filters.
- Start with over‑the‑counter antihistamines; move to topical steroids if needed.
- Cold compresses, oatmeal baths, and loose cotton clothing provide fast soothing.
- Consider immunotherapy if hives recur every season.
- Track flare‑ups in a simple diary to spot patterns and improve treatment.
Understanding Hives and Pollen Triggers
While the term “allergy” gets thrown around a lot, the specifics matter. Pollen microscopic grains released by trees, grasses, and weeds that can irritate the immune system is one of the most common culprits for seasonal hives. When your body mistakes pollen for a harmful invader, it releases histamine, a chemical that expands blood vessels and makes the skin leaky-hence the itchy welts.
Not everyone reacts the same way. Some people develop hives only after a high pollen count, while others may notice a flare‑up after just a short walk in a park. Knowing your personal threshold helps you plan activities and wardrobe choices better.
Immediate Relief Strategies
When a hive appears, rapid comfort is the priority. Below are the top five actions that work for most people:
- Cold Compress a bag of ice or chilled gel pack wrapped in a cloth - Apply for 10‑15 minutes to reduce swelling and numb the itch.
- Oatmeal Bath a warm soak with colloidal oatmeal that soothes irritated skin - Stay in for 15‑20 minutes; repeat twice a day if needed.
- Antihistamines oral medications that block histamine receptors - Non‑sedating options like loratadine or cetirizine work within an hour. Take as directed, even if you feel fine, to keep histamine levels low.
- Corticosteroid Cream topical steroids such as hydrocortisone 1% for localized relief - Apply sparingly to the worst spots; avoid prolonged daily use without a doctor’s guidance.
- Loose, breathable cotton clothing - Tight fabrics can trap heat and aggravate hives. Swap synthetic blends for cotton during high‑pollen days.
These measures often bring the itch down fast enough to let you get on with your day. Remember to wash your hands after applying any creams to prevent spreading the irritant.

Home Environment Adjustments
Even the best topical relief won’t solve the problem if pollen keeps streaming into your living space. Here’s how to create a hive‑friendly home:
- Air Purifier a device equipped with HEPA filters that capture pollen and other airborne particles - Place one in the bedroom and main living area. Change the filter every 3‑4 months for optimal performance.
- Keep windows and doors closed during peak pollen hours (usually early morning and late afternoon).
- Use a dehumidifier to maintain indoor humidity below 50%, which discourages dust mites and mold-additional allergens that can worsen hives.
- Shower and change clothes immediately after coming inside to rinse off pollen.
Lifestyle & Dietary Tweaks
Food doesn’t always cause hives, but certain dietary habits can amplify the body’s histamine response. Consider these adjustments:
- Stay hydrated - Water helps flush histamine out of the bloodstream. Aim for at least 2 L per day. \n
- Limit high‑histamine foods such as aged cheese, fermented soy, and wine during peak season.
- Incorporate natural anti‑inflammatory foods: ginger, turmeric, and omega‑3‑rich fish.
- Manage stress with short yoga sessions or breathing exercises; stress hormones can trigger histamine release.
Medical Options & When to Seek Help
If over‑the‑counter methods only provide temporary respite, it’s time to talk to a healthcare professional. Here’s what they might suggest:
- Prescription‑strength antihistamines or leukotriene inhibitors for stubborn cases.
- Short courses of oral steroids for severe, widespread hives (under strict medical supervision).
- Immunotherapy a long‑term treatment that gradually desensitizes the immune system to specific allergens - Involves regular allergy shots or sublingual tablets; can reduce or eliminate seasonal hives after 1‑3 years.
- Referral to a dermatologist or allergist for chronic urticaria that lasts beyond a few weeks.
Red flags that demand immediate medical attention include: swelling of the lips or throat, difficulty breathing, or hives accompanied by a fever. These could signal anaphylaxis, a life‑threatening emergency.

Treatment Options Comparison
| Option | Speed of Relief | Duration of Effect | Typical Cost (US) | Side‑Effects |
|---|---|---|---|---|
| Cold Compress | Immediate (minutes) | Short (30 min‑1 hr) | $0‑$5 (ice pack) | Skin irritation if applied too long |
| Antihistamine (OTC) | 30‑60 min | 12‑24 hr | $10‑$20 per month | Rare drowsiness (non‑sedating types avoid) |
| Corticosteroid Cream | 15‑30 min | Few hours | $5‑$15 per tube | Skin thinning with prolonged use |
| Immunotherapy (shots) | Weeks to months (gradual) | Years (disease‑modifying) | $1,000‑$3,000 annually | Local injection site reactions |
Prevention Checklist for Pollen Season
- Check local pollen count each morning (weather apps, allergy websites).
- Run an air purifier with a HEPA filter in bedroom.
- Keep windows shut during high‑pollen hours; use air‑conditioning on recirculate mode.
- Take a non‑sedating antihistamine before heading outdoors.
- Wear sunglasses and a wide‑brim hat to keep pollen off eyes and hair.
- Shower and change clothes immediately after returning home.
- Keep a diary of flare‑ups, noting weather, foods, stress levels, and medications.
Frequently Asked Questions
Can I use natural remedies instead of antihistamines?
Yes, many people find relief with cold compresses, oatmeal baths, and soothing creams. However, natural methods usually address symptoms rather than the underlying histamine surge. If your hives are frequent or severe, an antihistamine is often the most reliable first line.
How long should I wait before trying a prescription steroid?
Doctors typically reserve oral steroids for cases that don’t improve after a week of OTC antihistamines and topical treatments. Prolonged steroid use can cause serious side‑effects, so it’s a short‑term rescue, not a long‑term solution.
Is immunotherapy worth the cost?
For people who suffer from seasonal hives every year, immunotherapy can be a game‑changer. It targets the root cause-pollen sensitivity-so after 1‑3 years of regular shots, many report drastically fewer flare‑ups. The upfront cost is high, but the long‑term reduction in meds and doctor visits often balances out.
Do diet changes really help with hives?
While food isn’t the main driver for pollen‑related hives, some people have a secondary food‑histamine sensitivity. Cutting high‑histamine foods during peak pollen weeks can lower overall histamine load and make antihistamines work better.
When should I call emergency services?
If you notice swelling around the eyes, mouth, or throat, trouble breathing, wheezing, or a sudden drop in blood pressure, treat it as anaphylaxis. Use an epinephrine auto‑injector if prescribed and call 911 immediately.
By combining quick‑acting relief tricks, smart home adjustments, and a longer‑term plan with your doctor, you can keep the pollen from turning your skin into an itchy battlefield. Remember, the goal isn’t just to stop the rash today-it’s to enjoy the whole season without the constant scratch‑and‑scratch routine.

ashanti barrett
October 18, 2025 AT 21:56I get how miserable those welts can feel, especially when you’re trying to enjoy a sunny day. My first go‑to is a cold compress wrapped in a thin cloth – it numbs the itch fast. Pair that with a non‑sedating antihistamine taken before you head out and you’ll notice a big drop in flare‑ups. Also keep a spare pair of cotton socks handy; they’re breathable and won’t trap heat like synthetics.
Leo Chan
October 19, 2025 AT 17:23Hang in there, the season will pass and you’ve got tools to fight back! A quick oatmeal bath after a day outdoors can calm the skin like magic. Keep a portable air purifier in your car – it’s a game‑changer for unexpected pollen spikes.
jagdish soni
October 20, 2025 AT 12:49The article does a respectable job of cataloguing remedies but falls short of a true philosophical discourse on the nature of allergic response it merely scratches the surface of immunological nuance while presenting a checklist like a grocery list it could benefit from a deeper ontological exploration of histamine pathways.
Latasha Becker
October 21, 2025 AT 08:16The guide provides a solid foundation for managing pollen‑induced urticaria, but a few nuances warrant deeper scrutiny.
First, the reliance on OTC antihistamines assumes a uniform histamine blockade, which disregards inter‑individual cytochrome polymorphisms affecting drug metabolism.
Second, the suggested oatmeal baths, while soothing, may inadvertently alter skin pH, potentially compromising barrier function if performed excessively.
Third, the recommendation to “run an air purifier” lacks specificity regarding filter MERV ratings, which can dramatically influence efficacy against different pollen grain sizes.
Moreover, the omission of a stepwise escalation protocol-starting with a non‑sedating H1 antagonist, followed by a leukotriene receptor antagonist-creates a therapeutic vacuum for refractory cases.
It is also worth noting that scheduled antihistamine dosing prior to peak pollen exposure can attenuate the initial histamine surge, a prophylactic nuance absent from the checklist.
The table comparing treatment modalities accurately captures cost and speed, yet it fails to address patient‑reported outcome measures such as itch numeric rating scales.
From a mechanistic standpoint, immunotherapy’s capacity to induce regulatory T‑cell proliferation offers a disease‑modifying avenue far superior to mere symptom control.
Nevertheless, the financial barrier highlighted-$1,000 to $3,000 annually-should be contextualized within insurance reimbursement frameworks that vary by jurisdiction.
The dietary recommendations, while well‑intentioned, conflate histamine intolerance with pollen allergies, a distinction that could mislead readers.
Incorporating a brief food diary focusing on histamine load, separate from pollen exposure logs, would enhance self‑monitoring precision.
The brief note on stress management is apt; cortisol spikes can potentiate mast cell degranulation, thereby amplifying urticaria.
Finally, the emergency red‑flag section responsibly underscores anaphylaxis risk, but could be bolstered by a visual cue such as an emoji or icon for rapid scanning.
In sum, the guide is comprehensive yet would benefit from integrating pharmacogenomic considerations, clearer escalation algorithms, and patient‑centered outcome metrics.
Implementing these refinements can transform a good pamphlet into a best‑practice protocol for clinicians and sufferers alike.
parth gajjar
October 22, 2025 AT 03:43Honestly, every spring feels like a personal betrayal-my skin erupts like a battlefield and I’m left crying for a moment of peace.
The cold pack gives a fleeting relief, but the itch returns with vengeance.
Even the soothing oatmeal bath feels like a cruel joke when the welts keep multiplying.
Give me a cure, not just a band‑aid.
Maridel Frey
October 22, 2025 AT 23:09For those seeking a structured approach, consider maintaining a digital log that captures pollen count, medication timing, and symptom severity. This data can be shared with your allergist to fine‑tune the treatment plan. Additionally, schedule a quarterly review of your air purifier’s filter to ensure optimal performance.
Madhav Dasari
October 23, 2025 AT 18:36Hey folks, just a heads‑up: I swapped my regular tees for loose cotton shirts last season and the difference was night‑and‑day. Also, keep a spare bottle of non‑sedating antihistamine in your bag – you’ll thank yourself when the pollen hits hard. Stay chill and scratch‑free!
DHARMENDER BHATHAVAR
October 24, 2025 AT 14:03Start antihistamines early. Use a cold compress for 10 minutes. Keep windows closed during high pollen hours.
Kevin Sheehan
October 25, 2025 AT 09:29Allergies are a reminder of the body’s intricate balance, and when that balance tips, we feel the disruption keenly. By confronting the histamine surge head‑on, we assert control over a process that otherwise feels chaotic. The guide’s emphasis on prophylaxis is commendable, yet it invites us to question why we accept such discomfort as inevitable. A more aggressive stance-regular immunotherapy, vigilant monitoring-signals a refusal to be passive. In the end, the fight against hives mirrors the broader human struggle for agency.
Jay Kay
October 26, 2025 AT 03:56This article is okay but it’s missing the point. You don’t need every single product listed; you just need what works for you. Stop over‑complicating it. Focus on the basics and you’ll be fine.
Jameson The Owl
October 26, 2025 AT 23:23People think pollen is just a natural thing but there’s a hidden agenda behind the rise in seasonal hives the pharmaceutical industry pushes over‑the‑counter meds as a quick fix while ignoring the larger environmental manipulation that floods our air with engineered pollen the world doesn’t know it’s being altered for profit the government pretends to regulate but the loopholes are endless we need to look beyond the surface and question why our bodies are being targeted by unseen forces the solution isn’t more pills it’s awareness and self‑sufficiency
Rakhi Kasana
October 27, 2025 AT 18:49I’ve tried a few of the suggestions and the air purifier really helped on high‑pollen days. The oatmeal bath is soothing but I limit it to once a day to avoid drying my skin. Keeping a diary has uncovered that my flare‑ups also spike after stressful meetings. So a mix of environmental control and stress management seems key.
Sarah Unrath
October 28, 2025 AT 14:16Pollen sucks.
Liberty Moneybomb
October 29, 2025 AT 09:43Wow, that deep dive was intense – feels like the author just unlocked a secret level of allergy science! It’s almost conspiratorial how the “simple” tips hide layers of hidden knowledge. Suddenly I’m questioning every bottle of antihistamine I’ve ever taken. Maybe the real cure lies in a forbidden formula whispered by ancient herbalists. Either way, this post just blew my mind.
James Dean
October 30, 2025 AT 05:09It’s a solid reminder that prevention beats reaction every time. Tracking pollen and medication timing creates a feedback loop you can actually trust. Small steps add up to big relief.