Medical Education on Generics: Do Doctors Learn Drug Equivalence?
Doctors prescribe generics for 90% of all medications in the U.S., yet most never learned how to truly evaluate whether they work the same as brand-name drugs. It’s not that they don’t trust generics-it’s that they were never taught the science behind them.
What Bioequivalence Actually Means
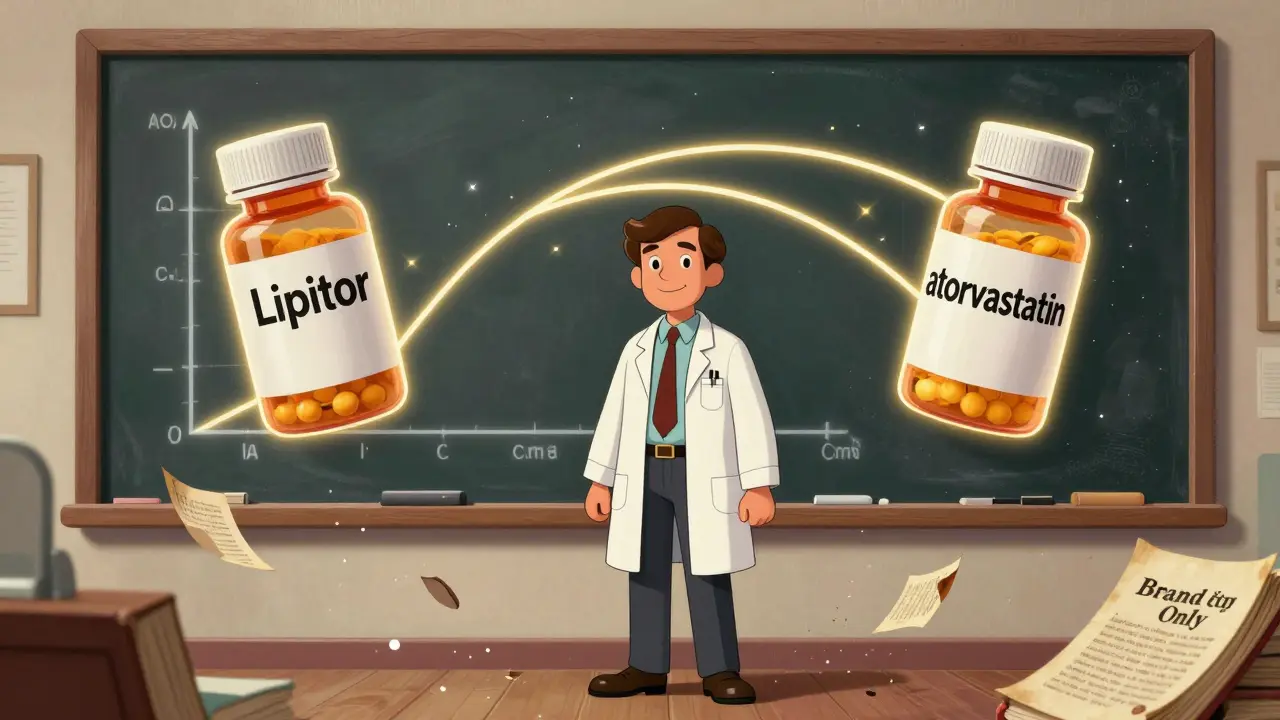
When a generic drug is approved by the FDA, it doesn’t just need to contain the same active ingredient as the brand-name version. It must prove bioequivalence: meaning it delivers the same amount of drug into the bloodstream at the same rate. That’s measured through two key numbers-AUC (area under the curve) and Cmax (peak concentration)-and both must fall within 80% to 125% of the brand drug’s values in healthy volunteers. This isn’t a guess. It’s a strict, statistically validated standard used worldwide by the FDA, EMA, and other agencies.
But here’s the problem: most medical students spend more time learning the mechanism of action for brand-name drugs like Lipitor or Prozac than they do on how generics are proven equivalent. A 2024 survey of U.S. medical schools found that pharmacology courses dedicated an average of 12 hours to brand-name drug mechanisms and just 28 minutes to generic substitution principles. That’s not an accident. Textbooks, case studies, and lectures overwhelmingly use brand names. One analysis from the AAMC showed 78% of clinical case examples still refer to brand names, even when generics are available. So by the time a doctor graduates, they’ve been trained to think in terms of brand names-not active ingredients.
Why Knowledge Doesn’t Translate to Practice
A 2015 study in Malaysia tested this gap head-on. They gave 30 doctors a 45-minute interactive lecture on bioequivalence, regulatory standards, and myths about generics. Afterward, their knowledge scores jumped from 58.7% to 84%. That’s a 25-point improvement. But when researchers looked at their actual prescribing habits six months later? Nothing changed. They still wrote prescriptions for brand-name drugs. Why?
Because knowledge alone doesn’t override culture. Junior doctors follow the habits of their seniors. If attending physicians always prescribe the brand, residents learn to do the same. It’s not about ignorance-it’s about routine. And when a patient asks why they’re getting a different pill, many doctors don’t have a clear, confident answer. A 2024 Medscape poll found that while 89% of physicians agreed generics are generally equivalent, only 54% felt completely confident explaining bioequivalence to patients. And just 31% regularly use International Nonproprietary Names (INN)-the generic drug names like “metformin” instead of “Glucophage.”
The Real Concerns Doctors Have
Some skepticism isn’t irrational. It comes from real experiences. In 2016, the FDA received dozens of reports from patients taking generic methylphenidate (Concerta) who said the medication didn’t work as well. The FDA investigated and confirmed all the generics met bioequivalence standards. But patients still felt different. Doctors like Dr. Lisa Chen on Doximity stopped automatically substituting after three patients reported reduced efficacy with the Teva version. Even though the science says it’s equivalent, the patient experience didn’t match.
That’s especially true for drugs with a narrow therapeutic index-where even small differences in blood levels can cause harm or reduced effect. Warfarin, levothyroxine, and certain antiepileptics fall into this category. A 2022 survey found 23.4% of neurologists were reluctant to switch epilepsy patients to generics. Psychiatrists and neurologists are the least likely to prescribe generics, with usage rates below 50%. Meanwhile, primary care doctors prescribe them 82% of the time. The difference? Exposure. Primary care sees more generic prescriptions, gets more feedback, and builds confidence through repetition.

What Actually Changes Behavior
Passive education-handouts, PDFs, one-time lectures-doesn’t work. A 2021 European study showed printed guidelines improved prescribing rates by only 7.2%. But something else did: feedback loops.
Pharmacist training studies show that reviewing 100 prescriptions with feedback helps trainees reach competence. The same applies to doctors. One family practice in Oregon started using the “teach-back” method: after prescribing a generic, they’d ask the patient, “Can you tell me why you’re getting this version instead of the brand?” Within months, patient questions about substitutions dropped by 63%. Why? Because the doctor had to explain it clearly-and the patient’s response revealed whether the explanation stuck.
Another effective tool: electronic health record alerts. When a doctor opens a prescription, a pop-up shows: “This generic meets FDA bioequivalence standards. Patient cost: $4 vs. $120.” Simple. Instant. At the point of decision. Only 38% of U.S. healthcare systems had these tools in 2022. But where they exist, generic prescribing jumps.
What’s Changing Now
The FDA launched its “Generic Drug Education for Healthcare Professionals” initiative in September 2023-15-minute microlearning modules on bioequivalence, free and online. The Agency for Healthcare Research and Quality (AHRQ) updated its prescribing guidelines in February 2024, strongly recommending INN use and teach-back. Karolinska Institute in Sweden started requiring INN prescribing in medical school evaluations in 2018. Graduates there now use generic names 47% more often.
By 2025, the FDA plans to integrate bioequivalence data directly into EHRs through its Digital Health Center of Excellence. Imagine: a doctor types “methylphenidate,” and the system shows a color-coded chart of all approved generics, their bioequivalence ranges, and patient reports-without leaving the prescription screen. That’s the future.
The Cost of Doing Nothing
Generics save the U.S. healthcare system $370 billion a year. They make up 90% of prescriptions but only 22% of drug spending. That’s not just money-it’s access. Patients who can’t afford brand-name drugs skip doses, delay treatment, or drop out of care entirely. But if doctors don’t feel confident prescribing generics, they won’t. And if patients don’t trust them, they won’t take them.
That’s why the real issue isn’t science. It’s communication. It’s training. It’s culture. We’ve proven generics work. But until medical education stops treating them as an afterthought-and starts teaching doctors how to explain, defend, and trust them-we’re leaving money, health, and lives on the table.
How to Start Fixing This
- Start with INN prescribing: Use metformin, not Glucophage. Lamotrigine, not Lamictal. Make it a habit in training.
- Use teach-back: Ask patients to explain why they’re getting a generic. It forces clarity and reveals misunderstandings.
- Push for EHR alerts: If your hospital doesn’t have them, ask for them. Simple prompts at the point of care change behavior faster than lectures.
- Watch your own prescribing: Track how often you write brand names vs. generics. You might be surprised.
- Use FDA resources: The agency offers free handouts and infographics on generic equivalence. Use them with patients.
The science is settled. The savings are real. The tools exist. What’s missing is the training-and the courage to change how we talk about it.
Do generic drugs work as well as brand-name drugs?
Yes, when approved by the FDA or EMA, generic drugs must prove bioequivalence-meaning they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. The FDA requires the 90% confidence interval for absorption (AUC) and peak concentration (Cmax) to fall between 80% and 125% of the brand drug’s values. This standard applies to all drug classes, including those with narrow therapeutic indexes like warfarin or levothyroxine. While inactive ingredients may differ, they do not affect safety or effectiveness.
Why do some doctors still prefer brand-name drugs?
Many doctors were trained using brand names in textbooks and case studies, which creates a strong habit. They may also have encountered rare patient reports of perceived reduced effectiveness-like the 2016 Concerta situation-despite regulatory confirmation of bioequivalence. Workplace culture plays a big role: if senior physicians prescribe brands, juniors follow. Lack of confidence in explaining bioequivalence to patients also leads to defaulting to familiar names.
Are there any drugs where generics aren’t safe to use?
No drug class is exempt from bioequivalence standards. Even for narrow therapeutic index drugs like antiepileptics, warfarin, or levothyroxine, the FDA requires the same 80-125% bioequivalence range. However, some specialists, like neurologists and psychiatrists, report higher reluctance to switch due to patient variability and past anecdotal reports. These concerns are real but not scientifically supported by regulatory data. The key is consistent formulation and close monitoring when switching-especially for drugs where small changes can have clinical effects.
How can medical schools improve generic drug education?
Medical schools should integrate bioequivalence into pharmacology courses with real-world examples, not just theory. Require use of International Nonproprietary Names (INN) in exams and case studies. Add interactive sessions with pharmacists who explain regulatory science. Use case-based learning where students compare brand and generic prescribing outcomes. One study showed a single 45-minute interactive lecture improved knowledge by 25 points. But lasting change requires reinforcement-feedback on prescribing patterns, EHR alerts, and longitudinal training.
What’s the most effective way to get patients to accept generics?
Use the teach-back method. Instead of just saying, “This is cheaper,” ask, “What do you understand about why we’re switching to this version?” This gives you a chance to correct misunderstandings and build trust. Pair it with simple, clear materials from the FDA-like patient handouts or bag stickers-that explain bioequivalence in plain language. Pilot programs showed patient acceptance of generics increased by 18.7% when providers used these tools consistently.
Is there data showing better outcomes when doctors prescribe generics?
Yes. Studies show patients on generics have better adherence because they’re more affordable. One analysis estimated that if all U.S. physicians prescribed generics confidently, the healthcare system could save $156 billion annually by 2030. In countries like Germany, where generic prescribing exceeds 90%, costs are lower and access is higher. The real barrier isn’t effectiveness-it’s perception. When doctors communicate clearly and consistently, patient trust and outcomes improve.
Doctors don’t need more lectures. They need better tools, clearer communication methods, and a system that supports them in making the right choice-not the familiar one.

Gregory Parschauer
January 14, 2026 AT 06:03Let me get this straight - we’re still having this conversation in 2025? Doctors are literally trained to treat generics like second-class citizens while charging patients $120 for a pill that’s $4 and *bioequivalent*. This isn’t ignorance, it’s institutionalized greed wrapped in a white coat. The FDA standards are rock solid. The science is settled. The only thing left to fix is the arrogance of physicians who’d rather keep their patients broke than admit they were never taught the basics.
Acacia Hendrix
January 14, 2026 AT 10:06It’s not merely a pedagogical oversight - it’s a structural epistemological failure in medical curricula. The hegemony of proprietary nomenclature reinforces a commodified pharmacological consciousness, wherein the active ingredient becomes ontologically subordinate to the brand as signifier. We’re not educating clinicians; we’re conditioning them to fetishize intellectual property under the guise of therapeutic fidelity.
Adam Vella
January 15, 2026 AT 15:00It is a well-documented phenomenon in medical education that exposure bias, reinforced by textbook authorship and clinical case selection, creates deeply entrenched cognitive heuristics. The fact that 78% of case studies still reference brand names, even when generics are available, is not incidental - it is systemic. The solution requires not only curricular reform but also a redefinition of clinical authority, wherein the prescriber is no longer the sole arbiter of therapeutic value but a conduit for evidence-based practice.
Nelly Oruko
January 16, 2026 AT 10:11So many docs think ‘bioequivalence’ means ‘close enough.’ It doesn’t. It means statistically identical absorption. The 80-125% range? That’s not a loophole - it’s a tight window proven safe across millions of patients. But if you’ve only ever heard ‘Lipitor’ since med school, your brain doesn’t even register ‘atorvastatin’ as the same thing. It’s like calling a cat a ‘meow machine’ because that’s all you’ve ever heard.
vishnu priyanka
January 17, 2026 AT 08:23In India, we use generics daily. No one blinks. We call it ‘sasta dawa’ - cheap medicine. But it works. My uncle takes generic warfarin for 10 years. His INR? Perfect. No drama. Maybe the problem isn’t the pill - it’s the American habit of turning medicine into a luxury brand. Why pay $120 when the same thing costs $4? Even our chaiwallahs know that.
Diana Campos Ortiz
January 18, 2026 AT 17:01I’m a nurse and I’ve seen patients cry because they can’t afford the brand. Then they get the generic, and they’re fine. One woman told me, ‘I thought it wouldn’t work, but my blood pressure’s better now.’ That’s the real story. Not the jargon. Not the lectures. Just a person getting better because someone finally trusted the science.
Jesse Ibarra
January 20, 2026 AT 09:15Anyone who still prescribes brand-name drugs out of habit is either a fraud or a coward. You think your patient’s ‘feeling different’ on generic Concerta? That’s placebo, not pharmacology. The FDA doesn’t lie. The 2016 reports were investigated. The generics passed. If you’re still scared, go back to med school. Or better yet - stop prescribing. Let someone who actually understands bioequivalence take over.
laura Drever
January 21, 2026 AT 03:18lol so the docs are just lazy? and the system is broken? yeah no shit. they teach brand names because its easier than learning 1000 generic names. and patients dont care as long as it works. so why fix it? capitalism wins again. 🤷♀️
Randall Little
January 21, 2026 AT 23:43Wait - you mean doctors don’t know their own job? Shocking. Next you’ll tell me plumbers don’t know what a pipe is. But seriously - if you’ve never had to explain why metformin isn’t ‘just some cheap version’ of Glucophage, you’ve been sheltered. The teach-back method? Genius. It turns the patient into the teacher. And suddenly, the doctor’s not the expert - they’re the translator.
Trevor Whipple
January 23, 2026 AT 23:18Bro, I’m a third-year med student and we spent 3 weeks on Lipitor but 20 minutes on atorvastatin. I had to google bioequivalence myself. My prof said ‘just prescribe the brand, it’s easier.’ So yeah, it’s not the docs’ fault - it’s the system. And now I’m gonna start using INNs on my rotations. Even if my attending hates it.