Mineral Bone Disorder in CKD: Understanding Calcium, PTH, and Vitamin D
What Is CKD-Mineral and Bone Disorder?
When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your bones and blood chemistry in balance. This isn’t just about weak bones. It’s a full-body problem called CKD-Mineral and Bone Disorder (CKD-MBD). It’s not a single disease. It’s a tangled web of broken signals between your kidneys, bones, parathyroid glands, and blood vessels. And it affects nearly everyone with moderate to severe chronic kidney disease (CKD).
By Stage 3, when kidney function drops below 60% of normal, your body starts sending warning signs. Phosphate builds up. Calcium drops. Vitamin D becomes inactive. Your parathyroid glands go into overdrive, pumping out too much PTH. Over time, this leads to brittle bones, calcified arteries, and a much higher risk of heart attack or fracture. The older term, "renal osteodystrophy," only talked about bone damage. CKD-MBD includes everything: bone, blood vessels, and the hormones that tie them together.
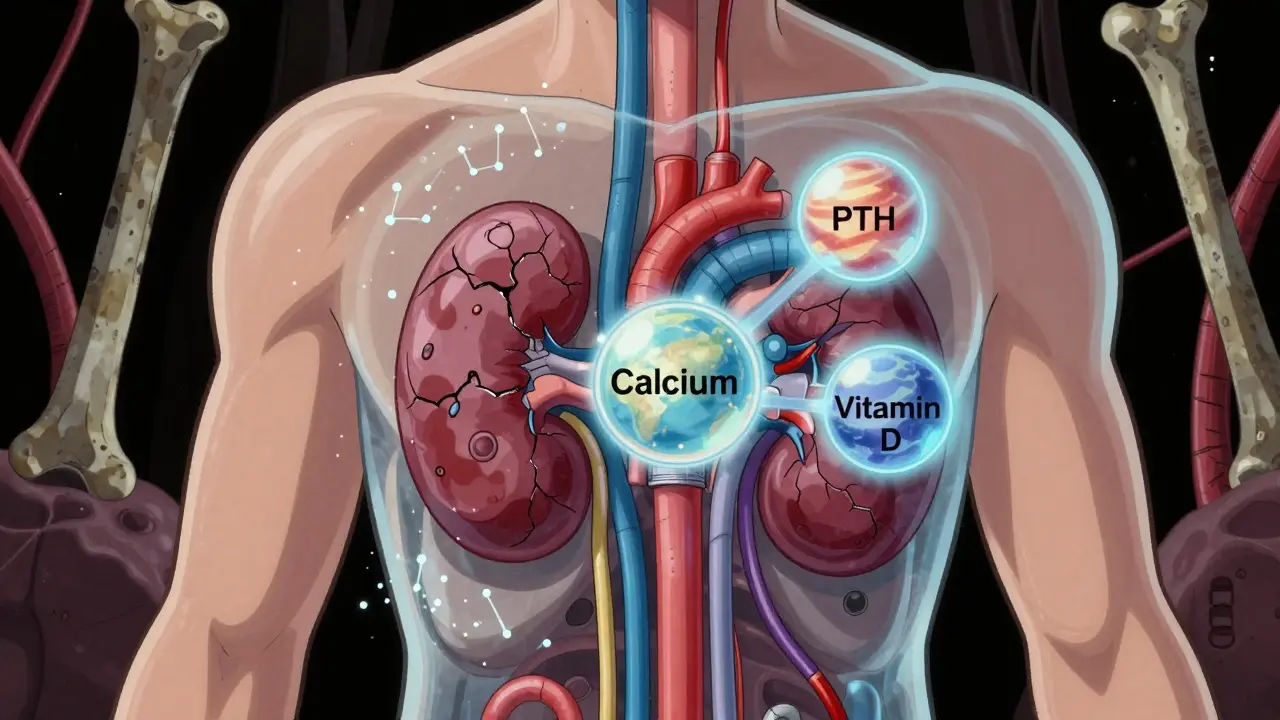
The Three Players: Calcium, PTH, and Vitamin D
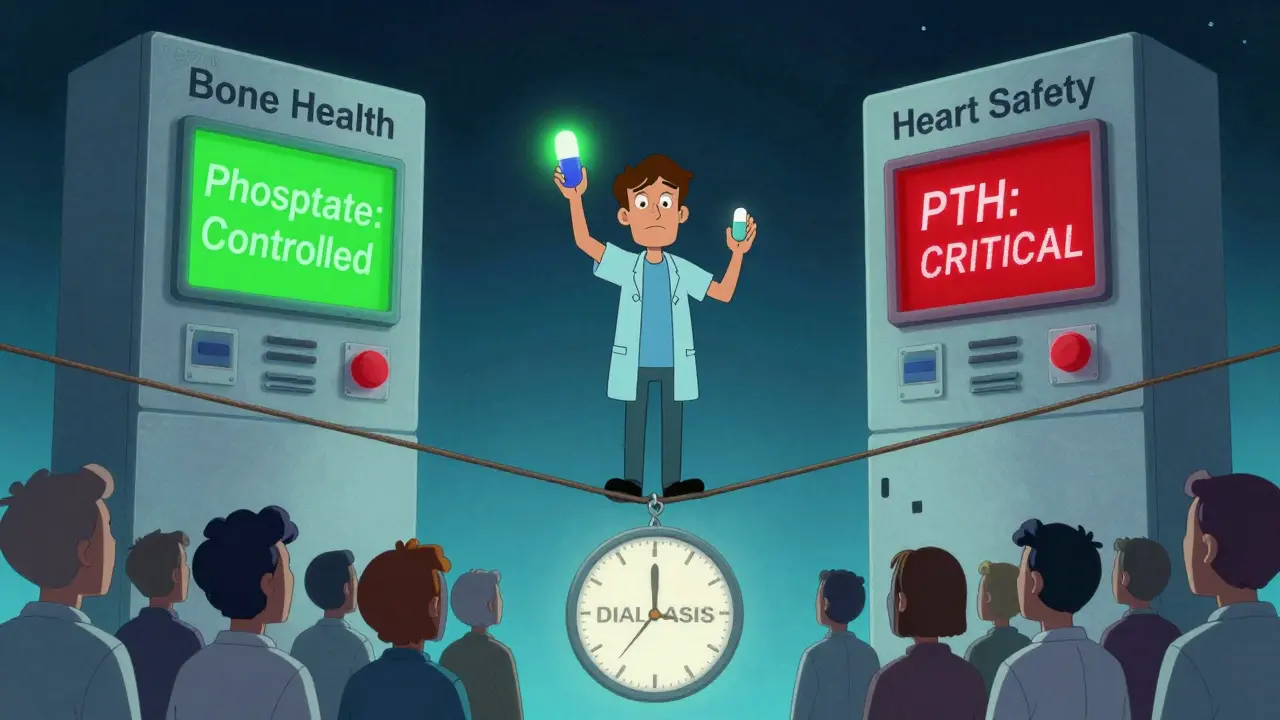
Think of your body as a tightrope walker balancing three weights: calcium, parathyroid hormone (PTH), and vitamin D. In healthy kidneys, these three stay in sync. In CKD, the balance collapses.
Calcium is the building block of bones and critical for muscle and nerve function. Healthy kidneys help keep blood calcium between 8.4 and 10.2 mg/dL. But when kidneys fail, they can’t activate vitamin D properly, which means your gut absorbs less calcium from food. Blood calcium drops. Your body panics.
PTH is the hormone your parathyroid glands release when calcium dips too low. It tells your bones to break down and dump calcium into your blood. In early CKD, PTH rises as a normal response. But over time, the glands grow larger and keep pumping out PTH even when it’s no longer helpful. Levels above 65 pg/mL in Stage 3, and over 300 pg/mL in dialysis patients, signal trouble. High PTH doesn’t just weaken bones-it also makes your blood vessels stiffen.
Vitamin D is the key that unlocks calcium absorption. Your kidneys convert inactive vitamin D (25(OH)D) into its active form, calcitriol. When kidneys fail, this conversion drops by 50-80%. That means even if you eat calcium-rich foods or take supplements, your body can’t use them. Eighty to ninety percent of people with Stage 3-5 CKD are deficient in vitamin D. And here’s the twist: taking regular vitamin D supplements can help. But giving active forms like calcitriol can backfire if phosphate is high, because it pushes calcium and phosphate even higher-making calcification worse.
How Phosphate Drives the Whole Cycle
Phosphate is the silent trigger. Healthy kidneys flush out excess phosphate. When kidney function drops below 40%, phosphate starts piling up. At first, you won’t feel it. But your body responds by releasing more FGF23, a hormone made by bone cells that tries to force the kidneys to pee out more phosphate. The problem? By Stage 4, your kidneys can’t respond anymore. FGF23 keeps rising, but now it starts attacking vitamin D production and even harms your heart.
High phosphate directly stimulates your parathyroid glands to make more PTH. It also binds to calcium in your blood, lowering free calcium even more. This creates a loop: low calcium → high PTH → bone breakdown → more phosphate released → more calcification. It’s self-sustaining. And it’s why phosphate control is the first line of defense.
What Happens to Your Bones?
Not all bone disease in CKD looks the same. There are three main patterns, and they’re not always easy to spot without a biopsy-which most people don’t get.
High turnover disease (osteitis fibrosa cystica) happens when PTH is sky-high-over 500 pg/mL. Your bones are constantly breaking down and rebuilding, but the new bone is weak. You’re at risk for fractures, bone pain, and deformities. This used to be the most common type, but it’s now less frequent thanks to better PTH control.
Low turnover disease (adynamic bone disease) is now the most common in dialysis patients-seen in 50-60% of cases. Here, PTH is too low (under 150 pg/mL). Bones barely rebuild at all. They look normal on scans, but they’re brittle. Fractures happen without trauma. This often results from over-treatment with vitamin D or calcimimetics, or from too much calcium in the blood.
Mixed disease is a combination of both. It’s harder to treat because you’re balancing two opposing problems at once.
One scary fact: dialysis patients have a 4-5 times higher risk of hip fracture than people their age without kidney disease. And many don’t even know they’re at risk because their bone density scans look normal.

Calcification: When Your Arteries Turn to Stone
Your bones aren’t the only thing turning brittle. Your arteries are calcifying-hardening like concrete. This is the hidden killer in CKD.
Up to 90% of dialysis patients show signs of vascular calcification on CT scans. Coronary arteries, heart valves, and even the skin can become stiff and narrow. This isn’t just plaque buildup. It’s calcium crystals forming in the walls of your blood vessels. And it’s directly linked to high phosphate, high PTH, and high calcium-phosphate product levels.
Every 1 mg/dL rise in serum phosphate increases your risk of dying by 18%. A 30% increase in PTH raises mortality risk by 12%. And if your calcium-phosphate product stays above 55, your risk of sudden cardiac death shoots up. Vascular calcification is responsible for about half of all deaths in people on dialysis.
Unlike cholesterol plaques, calcification doesn’t respond to statins. The only way to slow it is to control phosphate, calcium, and PTH-early and consistently.
How Is It Diagnosed?
You won’t feel CKD-MBD until it’s advanced. That’s why regular blood tests are non-negotiable.
Doctors track four key numbers:
- Phosphate: Target 2.7-4.6 mg/dL (Stages 3-5), 3.5-5.5 mg/dL (on dialysis)
- Calcium: 8.4-10.2 mg/dL
- PTH: 2-9 times the upper limit of normal (varies by lab, usually 150-600 pg/mL)
- 25-hydroxyvitamin D: At least 30 ng/mL
Bone biopsy is the gold standard for figuring out bone turnover, but it’s invasive and rarely done. Instead, doctors use blood markers like bone-specific alkaline phosphatase (BSAP) and PINP to guess what’s happening inside your bones. Vascular calcification is checked with X-rays or CT scans-especially if you have chest pain or high blood pressure.
Don’t wait for symptoms. If you have Stage 3 CKD or worse, you should have these tests every 3-6 months.
Treatment: It’s Not Just About Drugs
There’s no magic pill. Managing CKD-MBD means tackling phosphate, calcium, PTH, and vitamin D all at once.
Phosphate control starts with diet. Aim for 800-1,000 mg per day-no easy feat. Avoid processed foods, colas, and fast food. They’re loaded with hidden phosphate additives. Then, take phosphate binders with meals. Calcium-based binders (like calcium carbonate) work well but can add too much calcium. Non-calcium options like sevelamer or lanthanum are safer for your arteries but cost more.
Vitamin D: Start with nutritional vitamin D (cholecalciferol). Most people need 1,000-4,000 IU daily to reach 30 ng/mL. Only use active forms like calcitriol or paricalcitol if PTH is above 500 pg/mL-and only if phosphate is under control. Active forms can spike calcium and phosphate fast.
Calcium: Don’t overdo it. Keep total daily calcium (from diet + binders) under 1,500 mg. Aluminum-based binders are banned in most places because they cause brain toxicity.
PTH control: If PTH stays high despite other treatments, calcimimetics like cinacalcet or etelcalcetide can help. These drugs trick the parathyroid gland into thinking calcium is higher than it is, so it stops overproducing PTH. Etelcalcetide, given as a weekly IV, reduces PTH by 45% in trials-better than the older oral option.
And here’s the biggest shift in thinking: you don’t treat numbers. You treat the whole system. Lowering phosphate alone won’t help if you’re giving too much active vitamin D. Reducing PTH too much can cause adynamic bone disease. It’s a tightrope walk.
What’s New in 2025?
Research is moving fast. A new class of drugs called anti-sclerostin antibodies (like romosozumab) is being tested. These drugs block a protein that stops bone formation. In early trials, they increased bone density by 30-40% in CKD patients without raising phosphate. That’s huge.
Scientists are also looking at Klotho, a protein made by kidneys that helps FGF23 work properly. In CKD, Klotho drops by 50-70%. Animal studies show that giving Klotho reduces calcification and improves bone strength. Human trials are coming.
And the guidelines are changing. The 2024 KDIGO draft recommends starting phosphate and vitamin D monitoring as early as Stage 3 CKD-not just when you’re on dialysis. Why? Because FGF23 rises 5-10 years before phosphate does. Early intervention could prevent the whole cascade.
What You Can Do Today
If you have CKD, here’s your action list:
- Get your phosphate, calcium, PTH, and vitamin D levels checked every 3-6 months.
- Ask your doctor if you’re on the right type of phosphate binder. Avoid calcium-based ones if your calcium is already high.
- Take nutritional vitamin D (D3), not active forms, unless your PTH is very high.
- Read food labels. Avoid ingredients with "phos" in them-phosphate additives are everywhere.
- Don’t assume your bone density scan is enough. Low turnover disease looks normal on scans but is just as dangerous.
- Ask about calcimimetics if your PTH is over 800 pg/mL and you’re still having bone or heart issues.
CKD-MBD isn’t something you fix once. It’s a lifelong balancing act. But with the right care, you can protect your bones, your heart, and your future.
Frequently Asked Questions
Can vitamin D supplements help with CKD-MBD?
Yes-but only the right kind. Nutritional vitamin D (cholecalciferol or ergocalciferol) helps raise low 25(OH)D levels and is safe for most people with CKD. It’s linked to a 15% lower risk of death. But active forms like calcitriol or paricalcitol should only be used if PTH is very high and phosphate is under control. These can raise calcium and phosphate dangerously if used too early or too much.
Why is phosphate so dangerous in kidney disease?
When kidneys fail, they can’t remove phosphate from your blood. High phosphate triggers your parathyroid glands to release more PTH, which pulls calcium from your bones. It also causes calcium and phosphate to deposit in your blood vessels, making them stiff and prone to rupture. Each 1 mg/dL rise in phosphate increases your risk of death by 18%. That’s why controlling phosphate is the most important step in preventing heart disease and fractures.
Can CKD-MBD cause fractures even if my bones look normal on a scan?
Absolutely. The most common bone problem in dialysis patients today is adynamic bone disease-where bone turnover is so low that new bone barely forms. Your bone density scan may look normal, but your bones are brittle and weak. This type of fracture happens without trauma, often in the hip or spine. It’s silent until it happens.
Are phosphate binders necessary if I eat a low-phosphate diet?
Yes, most people still need them. Even with a strict low-phosphate diet, your body absorbs phosphate from processed foods, medications, and even supplements. Phosphate binders are taken with meals to trap phosphate in your gut so it doesn’t enter your blood. Without them, it’s nearly impossible to keep phosphate under control, especially as kidney function declines.
Can I take calcium supplements if I have CKD?
Only if your doctor says so-and even then, be careful. Calcium supplements can raise your blood calcium and increase the risk of vascular calcification. Most people get enough calcium from food. If you need more, your doctor may recommend calcium-based phosphate binders instead of standalone supplements. Total daily calcium intake (from food + binders) should not exceed 1,500 mg.

Jennifer Taylor
December 16, 2025 AT 21:26Shelby Ume
December 17, 2025 AT 17:56Jade Hovet
December 18, 2025 AT 22:28nithin Kuntumadugu
December 19, 2025 AT 05:42John Fred
December 19, 2025 AT 12:45Harriet Wollaston
December 21, 2025 AT 03:59Lauren Scrima
December 21, 2025 AT 10:31Himmat Singh
December 21, 2025 AT 23:06Alvin Montanez
December 22, 2025 AT 01:56Lara Tobin
December 23, 2025 AT 01:25Jamie Clark
December 23, 2025 AT 17:15Keasha Trawick
December 25, 2025 AT 09:16Bruno Janssen
December 27, 2025 AT 00:32Jennifer Taylor
December 28, 2025 AT 04:15