Severe Hyponatremia from Medications: Signs, Risks, and What to Do

Hyponatremia Risk Assessment Tool
What is hyponatremia?
Hyponatremia is a dangerous condition where your blood sodium level drops below 135 mmol/L. Severe cases can cause brain swelling, seizures, confusion, and even coma within hours. It's often overlooked as a side effect of common medications.
When your sodium levels drop too low, your brain starts to swell. It’s not a slow, gentle process-it can happen in hours. And for many people taking common medications, this isn’t rare. Hyponatremia from drugs is one of the most dangerous, yet overlooked, side effects in modern medicine. It doesn’t always show up as a lab anomaly on a routine blood test. Often, it shows up as confusion, nausea, or a sudden seizure-and by then, it’s already an emergency.
What Exactly Is Hyponatremia?
Hyponatremia means your blood sodium level is below 135 mmol/L. Severe cases drop below 120 mmol/L. Sodium isn’t just about salt on your food. It’s the key electrolyte that keeps your cells balanced, especially your brain cells. When sodium drops too fast, water rushes into your brain to even things out. Your brain doesn’t have room to expand. It gets squeezed. That’s when confusion, seizures, and coma start.Which Medications Cause It?
Not all drugs cause this. But some do-often quietly, without warning. The biggest culprits:- SSRIs (like sertraline, citalopram, fluoxetine): These antidepressants trigger SIADH-where your body holds onto too much water. About 22% of drug-induced hyponatremia cases come from these.
- Diuretics (especially thiazides like hydrochlorothiazide): These make you pee out sodium. They’re responsible for nearly 30% of cases.
- Antiepileptics (carbamazepine, oxcarbazepine): These can drop sodium by 0.5 to 1.0 mmol/L per day. One patient’s sister had a seizure on oxcarbazepine. Her pharmacist caught it before she started-her sister didn’t.
- MAOIs, ACE inhibitors, NSAIDs: Less common, but still dangerous, especially in older adults.
- MDMA (ecstasy): Even recreational drugs can cause this. People don’t realize it’s not just dehydration-it’s water intoxication.
It’s not about taking one pill. It’s about who’s taking it. People over 65 are 2.7 times more likely to develop it. Women are more at risk than men. And if you’re on more than one of these drugs? Your risk jumps.
How Fast Does It Happen?
This isn’t something that builds over months. It’s fast. Most severe cases show up within 1 to 4 weeks after starting the drug. In 73% of cases, sodium drops below dangerous levels within the first 30 days. That’s why monitoring matters.One nurse on Reddit described a 72-year-old patient who started sertraline. Within 10 days, sodium dropped from 138 to 118 mmol/L. The doctor called the early nausea and headaches “normal side effects.” Then the patient had a grand mal seizure. That’s not rare. It’s predictable.
What Are the Warning Signs?
The symptoms are easy to miss because they look like other things:- Confusion (happens in 68% of severe cases)
- Headaches (often dismissed as tension or stress)
- Nausea or vomiting (called “flu-like”)
- Muscle weakness or cramps
- Seizures (22% of cases when sodium is below 115 mmol/L)
- Coma (if untreated)
Over 68% of patients in patient forums say they were first misdiagnosed. “Flu.” “Anxiety.” “Early dementia.” One woman spent weeks in therapy for “depression” while her sodium kept dropping. Her blood test finally caught it.
Why Is This So Dangerous?
Your brain adapts slowly to low sodium. But when it drops fast-like from a new medication-it doesn’t have time to adjust. The swelling happens too quickly. That’s when brain damage starts. And if sodium is corrected too fast later? You risk a different disaster: osmotic demyelination syndrome. That’s when the brain’s protective coating gets ripped off. It can leave you locked-in, unable to speak or move.Doctors know this. But many still rush correction. The European Society of Endocrinology says: correct no more than 6 mmol/L in 24 hours. The American Society of Nephrology says up to 8-10 mmol/L is okay with close monitoring. Either way, it’s not a DIY fix. It needs hospital care.
Who’s at Highest Risk?
- People over 65: 61% of severe cases
- Women: 57% of cases
- Those on multiple high-risk drugs: Like an SSRI + a diuretic
- People with heart failure, kidney disease, or thyroid problems
It’s not about being “weak” or “fragile.” It’s about biology. Older adults have less kidney reserve. Women have higher levels of antidiuretic hormone. These aren’t accidents. They’re physiological realities.
How Is It Diagnosed?
It’s not hard-but it’s often missed. A simple blood test: serum sodium. If it’s below 135, you’re in the danger zone. If it’s below 125, you need urgent care. But labs don’t flag it unless someone orders it.The key is suspicion. If you start a new medication and feel weird within 2 weeks-get your sodium checked. No waiting. No “see how it goes.”
There’s a tool called the Hyponatremia Algorithm from the European Hyponatremia Network. It’s used in hospitals and cuts misdiagnosis from 31% to under 11%. But it only works if doctors use it.
What’s the Treatment?
It depends on how fast the sodium dropped and how low it is.- Severe symptoms (seizures, coma): Hospital. IV saline. Close monitoring. No fast fixes.
- Mild to moderate: Stop the drug. Fluid restriction. Sometimes, salt tablets.
- New option since 2023: Tolvaptan (Samsca). It helps your kidneys flush out water without losing sodium. It’s been shown to correct sodium 34% faster than standard care.
But here’s the catch: if you need the drug-for depression, seizures, or high blood pressure-you can’t just quit it. That’s why recurrence is so common. 33% of people on SSRIs get hyponatremia again, even after stopping and restarting. That’s why alternatives matter.

Can It Be Prevented?
Yes. But only if we change how we prescribe.- Check sodium before starting high-risk drugs-especially in older adults.
- Check again within 7 days after starting. Then every 3-5 days for the first month.
- Pharmacists should warn patients. Since March 2024, the EMA requires pharmacists to explain sodium risk at pickup for drugs like carbamazepine and SSRIs.
- Ask: “Could this be low sodium?” before writing off symptoms as “side effects.”
One Mayo Clinic patient said their pharmacist caught a dangerous interaction between oxcarbazepine and hydrochlorothiazide before they filled the prescription. “Saved me from what happened to my sister.” That’s not luck. That’s protocol.
Why Isn’t This Done More Often?
Because we’re still treating symptoms, not causes. Only 63% of doctors follow the FDA’s 2022 warning to monitor sodium in the first 30 days. Community clinics do it 47% of the time. Academic hospitals? 82%. That gap kills people.Dr. Robert Stern put it bluntly in JAMA: “Why aren’t we mandating sodium checks for every patient starting an SSRI or thiazide?” The answer? Cost. Time. Habit. But the cost of a missed diagnosis? A hospital stay. A seizure. A lifetime of disability. It’s $473 million a year in the U.S. alone.
What’s Next?
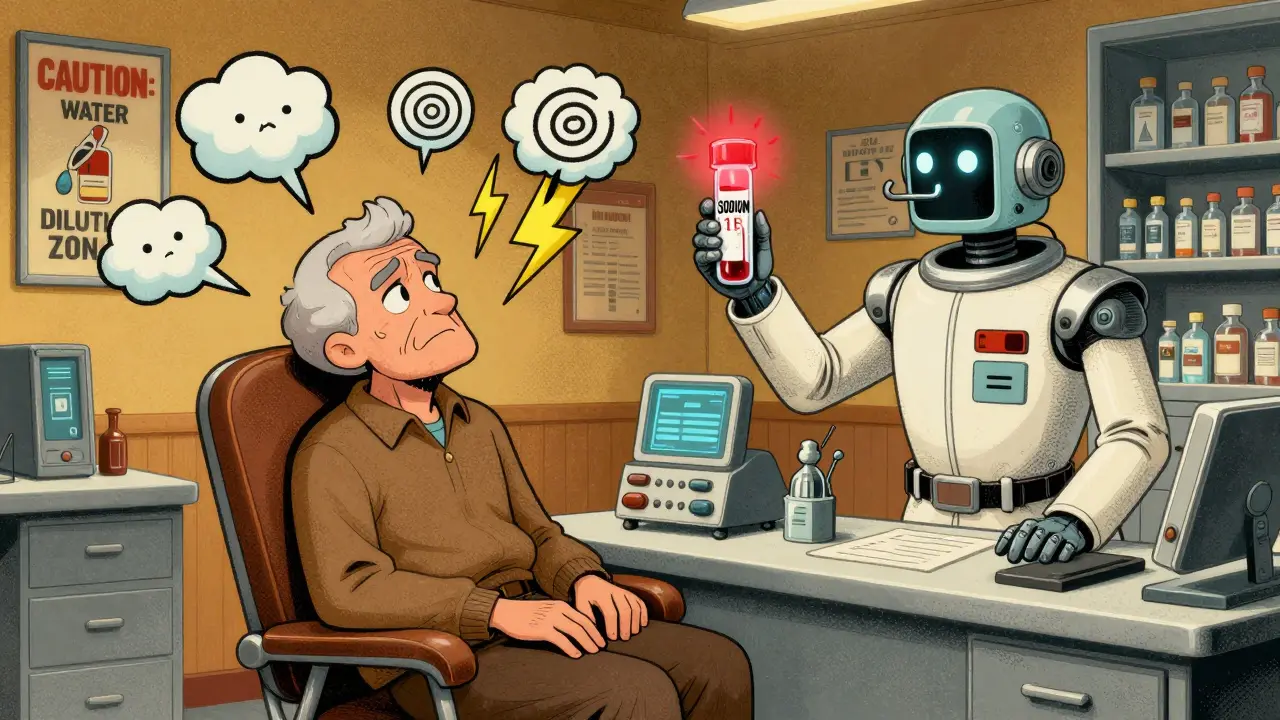
AI is stepping in. Mayo Clinic’s algorithm analyzes EHR data-meds, age, labs, symptoms-and predicts hyponatremia 72 hours before it happens. Accuracy? 87%. It’s not in every clinic yet. But it will be.By 2028, cases will rise 22% as the population ages. But if we start checking sodium routinely-especially in the first 30 days of high-risk meds-we could cut severe complications by 38%.
The window between confusion and seizures? As short as 6 to 8 hours. You don’t get a second chance if you wait.
What Should You Do?
- If you’re on an SSRI, diuretic, or antiepileptic: Ask your doctor for a sodium test. Now.
- If you’ve had nausea, headaches, or confusion since starting a new med: Don’t wait. Get tested.
- If you’re a caregiver for an older adult: Watch for sudden changes in behavior. It’s not dementia. It could be low sodium.
- If you’re a pharmacist or nurse: Don’t assume someone else will check. Flag it.
Hyponatremia isn’t rare. It’s predictable. And it’s preventable-if we start looking for it.
Can antidepressants cause low sodium?
Yes. SSRIs like sertraline, citalopram, and fluoxetine are among the top causes of medication-induced hyponatremia. They trigger SIADH, a condition where the body holds onto too much water, diluting sodium in the blood. About 22% of all drug-related hyponatremia cases come from SSRIs. Symptoms like nausea, confusion, or headaches within the first few weeks of starting the drug should prompt a sodium blood test.
How long does it take for hyponatremia to develop from medication?
It usually develops within 1 to 4 weeks after starting the medication. In fact, 73% of severe cases occur within the first 30 days. That’s why checking sodium levels within 7 days of starting high-risk drugs like diuretics or SSRIs is critical. Sodium can drop as fast as 0.8 mmol/L per day-fast enough to cause seizures before most people realize something’s wrong.
Can hyponatremia be reversed?
Yes-if caught early. When treatment starts within 24 hours of symptoms, recovery rates are 92%. But if treatment is delayed beyond 48 hours, recovery drops to 67%. The key is not just correcting sodium, but doing it slowly. Rapid correction can cause osmotic demyelination syndrome, leading to permanent brain damage. Treatment usually involves stopping the drug, fluid restriction, and sometimes IV saline or tolvaptan under medical supervision.
Is hyponatremia from drugs more dangerous than other causes?
It’s not necessarily more dangerous, but it’s more sudden. Medication-induced hyponatremia often drops sodium rapidly, giving the brain no time to adapt. That’s why seizures and confusion appear faster than in chronic cases like heart failure or kidney disease. The good news? It’s often reversible when the drug is stopped and sodium is corrected properly. But if ignored, the risk of death or permanent brain injury is just as high as with any other cause.
What should I do if I think I have low sodium from my meds?
Don’t wait. Contact your doctor immediately and ask for a serum sodium blood test. If you have seizures, confusion, or vomiting, go to the emergency room. Don’t assume it’s the flu, anxiety, or aging. Early detection saves lives. If you’re on an SSRI, diuretic, or antiepileptic drug and feel off, get tested. It takes 5 minutes. The consequences of waiting could be permanent.
Are there any new treatments for drug-induced hyponatremia?
Yes. In November 2023, the FDA approved tolvaptan (Samsca) specifically for medication-induced hyponatremia. It works by helping the kidneys excrete water without losing sodium. Clinical trials showed it corrects sodium levels 34% faster than standard fluid restriction. It’s not for everyone-it requires monitoring-but it’s a major step forward. Also, since March 2024, European guidelines require pharmacists to educate patients about sodium risk when dispensing high-risk drugs.

Margaret Khaemba
January 23, 2026 AT 05:54I had no idea SSRIs could do this. My mom started on sertraline last year and kept saying she felt "off"-headaches, nausea, like the flu. We just thought it was adjusting. Now I’m freaking out and asking her doctor for a sodium test tomorrow. This post saved me from a potential disaster.
Chiraghuddin Qureshi
January 24, 2026 AT 09:34Bro this is wild 🤯 I’m on carbamazepine for seizures and my doc never mentioned this. Gonna get my sodium checked ASAP. India’s healthcare is so behind on this stuff. Thanks for the heads up!
Lauren Wall
January 24, 2026 AT 10:58Doctors are negligent. Period. This is preventable. If you’re on these meds and feel weird, demand a blood test. No excuses.
Lana Kabulova
January 25, 2026 AT 17:32So let me get this straight-you’re telling me my antidepressant could literally make me seize because my doctor didn’t check my sodium? I’ve been on citalopram for 11 months. I’ve had constant headaches since day one. They called it "anxiety." I’m 52. Female. On a diuretic too. I’m not "just tired." I’m being slowly poisoned. And no one cared. I’m going to the ER tomorrow. I’m not waiting.
shivani acharya
January 27, 2026 AT 13:00Oh wow, so the pharmaceutical companies are just letting people get brain damage because they don’t want to pay for lab tests? And now they’ve got this "tolvaptan" drug that fixes it but costs $800 a month? Classic. They make the problem, then sell you the expensive fix. And the FDA? They’re in bed with Big Pharma. That’s why they only require pharmacists to warn people in Europe. Here? You’re on your own. My cousin’s husband died from this. They said "heart failure." It was hyponatremia from hydrochlorothiazide. No one ever asked if he was on meds. Just assumed he was old. He was 61.
Alec Amiri
January 29, 2026 AT 12:23Y’all are overreacting. I’ve been on hydrochlorothiazide for 10 years. I’m fine. You’re all panic-scrolling. Just drink more water and stop being hypochondriacs. Also, SSRIs? They’re life-saving. Don’t throw the baby out with the bathwater.
Patrick Roth
January 30, 2026 AT 05:34Actually, the 22% stat for SSRIs is misleading. Most of those cases are in elderly polypharmacy patients. In healthy adults under 50? The risk is basically zero. Also, tolvaptan isn’t FDA-approved for this indication-it’s off-label. You’re scaring people with cherry-picked data. The real danger is people stopping their meds because of fear-mongering.
Kenji Gaerlan
January 31, 2026 AT 04:23wait so u mean like if u take an antidep and get a headache its not just stress? but like brain swelling? wow i never thought of that. i think i might have this. i started sertraline 3 weeks ago and i keep feeling dizzy. should i go to er? or just wait?
Tatiana Bandurina
January 31, 2026 AT 04:28It’s interesting how this is framed as a medical failure, but the real issue is systemic underfunding of primary care. If doctors had 30 minutes per patient instead of 7, they’d order the labs. But they don’t. And patients don’t push back because they’ve been conditioned to trust authority. So we get this: preventable tragedies disguised as "unfortunate complications."
Ryan Riesterer
February 1, 2026 AT 10:35The pathophysiology here is textbook: SIADH from SSRI-induced ADH dysregulation. The real clinical takeaway is the temporal window-72 hours post-initiation is the critical monitoring period. The 2023 Mayo AI model has an AUC of 0.91 for predicting hyponatremia within 7 days of SSRI initiation. Validation cohort: n=12,000. This isn’t anecdotal-it’s evidence-based. The lag in adoption is a systems problem, not a knowledge gap.
Akriti Jain
February 1, 2026 AT 20:44They’re hiding this on purpose. Why do you think the FDA didn’t mandate testing until 2022? Because the drug companies don’t want you to know you can get brain damage from a pill you take for anxiety. And now they’ve got this "new treatment"-totally overpriced, patented, and only available if you’re rich. Meanwhile, your grandma in a nursing home is getting sertraline and hydrochlorothiazide together. And they say "it’s just aging." 😏
Mike P
February 3, 2026 AT 09:22Look, America’s healthcare is broken. We let pharma run the show. In Canada, they check sodium before you even get the script for an SSRI. Here? You gotta beg. I’m a veteran. I got mine through the VA-they tested me. My doc said "good catch." I’m alive because they didn’t assume I was fine. Shame on the rest of the system.
Jasmine Bryant
February 4, 2026 AT 04:18Just wanted to say thank you for posting this. I’m a nurse in a rural clinic and I’ve seen this happen twice. One guy on fluoxetine and HCTZ-sodium dropped to 116. He had a seizure in the waiting room. We didn’t even know he was on both. Now I check sodium on every new SSRI or diuretic patient over 60. It takes 2 minutes. It’s worth it.
Liberty C
February 6, 2026 AT 01:05It’s tragic that we’ve turned medicine into a lottery. You either get a doctor who cares enough to order a basic blood test-or you get a corpse. And the worst part? The people who die from this are the ones who trusted the system. They didn’t google symptoms. They didn’t panic. They just took their pills and hoped for the best. Meanwhile, the pharmaceutical industry is quietly counting their billions. This isn’t negligence-it’s commodification of human biology.