Alcohol and Diabetes: How Drinking Affects Blood Sugar and Medication Safety
When you have alcohol and diabetes, the interaction between drinking and blood sugar control can be unpredictable and dangerous. Also known as alcohol-induced hypoglycemia, this isn’t just about feeling dizzy after a beer—it’s about your body’s ability to regulate glucose when alcohol is in the system. Alcohol blocks the liver from releasing stored sugar, which can cause your blood sugar to drop dangerously low, especially if you’re taking insulin or pills like sulfonylureas. This risk doesn’t go away after you stop drinking—it can last for hours, even overnight.
People with diabetes medication interactions, how certain drugs react with alcohol need to be extra careful. Metformin, for example, already carries a small risk of lactic acidosis, and alcohol increases that risk. Glipizide or glyburide can cause severe lows if mixed with even one drink. And if you’re using insulin? Drinking without eating can turn a night out into an emergency. It’s not about quitting entirely—it’s about knowing when, how much, and how to protect yourself. The American Diabetes Association says moderate drinking (one drink per day for women, two for men) is okay for most, but only if your blood sugar is stable and you eat with it.
blood sugar control, the process of keeping glucose levels steady gets messy with alcohol because it hides the signs of low blood sugar. Shakiness, sweating, dizziness—those feel like being drunk. But they’re also the same symptoms of hypoglycemia. If you’re out and your glucose drops, you might not realize it until it’s too late. That’s why checking your levels before, during, and after drinking matters more than ever. Carry fast-acting sugar like glucose tabs, wear a medical ID, and tell someone you’re with that you have diabetes.
Some people think skipping their diabetes meds before drinking is safer. It’s not. Missing doses leads to high blood sugar, and then drinking on top of that creates a rollercoaster. Others avoid alcohol completely, which works—but if you choose to drink, you need a plan. Eat protein and carbs with your drink. Avoid sweet cocktails and beer, which pack hidden sugars. Stick to dry wine, light beer, or spirits with soda water. And never drink on an empty stomach.
There’s no one-size-fits-all rule, but the data is clear: alcohol changes how your body responds to diabetes treatment. It affects your liver, your nerves, your weight, and even your judgment about food and meds. That’s why so many posts here focus on real risks—like how metronidazole and garlic supplements can interact with other meds, or how lab monitoring helps catch problems early. You’re not alone in this. People with diabetes manage alcohol safely every day. It’s not about fear—it’s about awareness, preparation, and knowing your own limits. Below, you’ll find detailed guides on how specific medications behave around alcohol, what to watch for, and how to adjust your routine without giving up everything you enjoy.
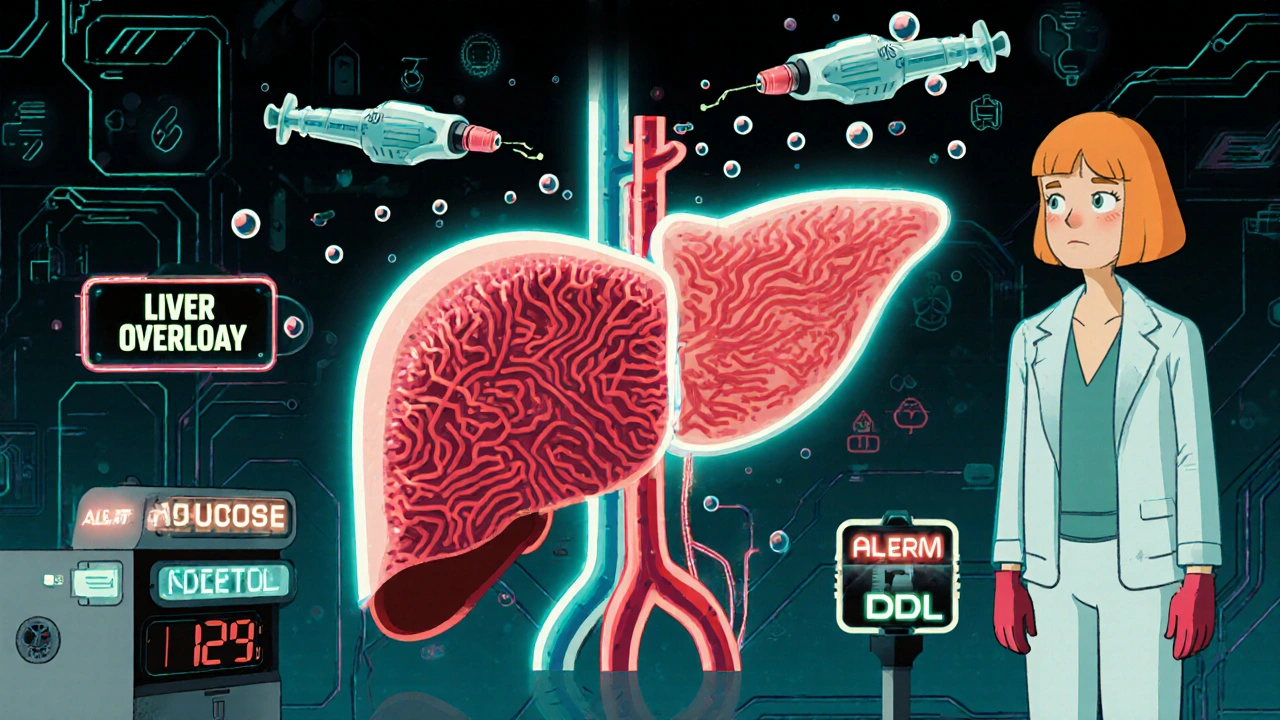
Alcohol and Diabetes Medications: How Alcohol Causes Low Blood Sugar and Liver Stress
Alcohol can cause dangerous drops in blood sugar when taken with diabetes meds like insulin or metformin. Learn how it affects your liver, why symptoms are hard to spot, and what steps to take if you choose to drink.
