Diabetes Medications Side Effects: What You Need to Know Before Taking Them
When you’re managing diabetes medications, prescription drugs used to control blood sugar in people with type 1 or type 2 diabetes. Also known as antihyperglycemic agents, these drugs help prevent complications—but they don’t come without risks. Many people assume that because these medications are prescribed, they’re harmless. But diabetes medications side effects are common, sometimes serious, and often overlooked.
Take metformin, the first-line drug for type 2 diabetes that reduces liver glucose production. Also known as Glucophage, it’s widely used because it’s cheap and doesn’t cause weight gain. But up to 25% of users get stomach upset, diarrhea, or nausea—especially when starting out. Some even develop vitamin B12 deficiency over time, which can lead to nerve damage if unchecked. Then there’s insulin, a hormone therapy that forces cells to absorb glucose. Also known as basal or bolus insulin, it’s life-saving for type 1 diabetics, but it can drop blood sugar too low. Hypoglycemia isn’t just dizziness or sweating—it can cause seizures, loss of consciousness, or even death if not treated fast.
Other drugs like sulfonylureas and SGLT2 inhibitors carry their own risks. Sulfonylureas can trigger weight gain and low blood sugar. SGLT2 inhibitors, while great for heart and kidney protection, have been linked to rare but dangerous genital infections and a condition called euglycemic diabetic ketoacidosis—where blood sugar isn’t high, but the body is still in acid crisis. Even newer drugs like GLP-1 agonists, which help with weight loss, can cause nausea, vomiting, or pancreatitis in rare cases. And let’s not forget drug interactions. A supplement like garlic, which some diabetics take to lower blood sugar, can make metformin or insulin work too well—and that’s when things get dangerous.
What most people don’t realize is that side effects aren’t random. They’re predictable. And they’re manageable—if you know what to look for. Lab monitoring, tracking symptoms, and knowing when to call your doctor can turn a risky situation into a safe one. You don’t have to suffer through nausea or panic over low blood sugar. The tools to protect yourself are already out there.
Below, you’ll find real, detailed breakdowns of how these drugs affect people in practice. From the quiet dangers of long-term metformin use to the hidden risks of combining insulin with certain foods or supplements, these posts give you the facts without the fluff. No marketing. No guesswork. Just what actually happens when you take these medicines—and how to stay in control.
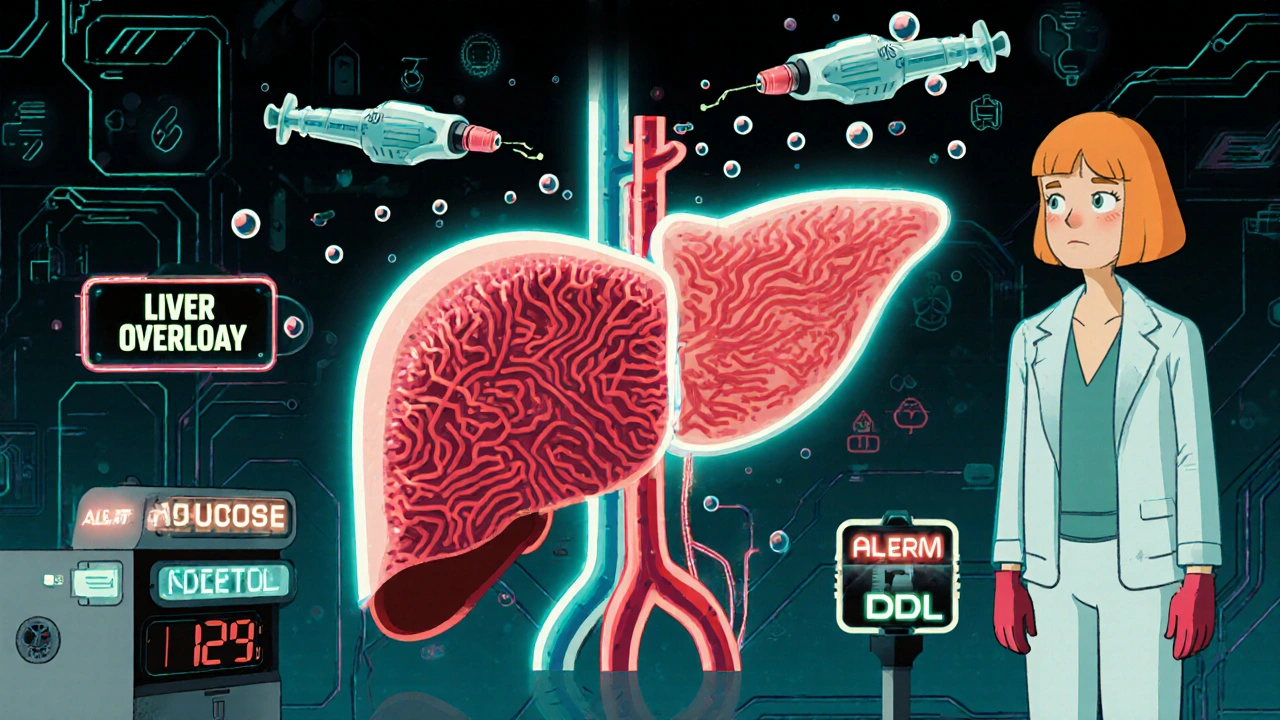
Alcohol and Diabetes Medications: How Alcohol Causes Low Blood Sugar and Liver Stress
Alcohol can cause dangerous drops in blood sugar when taken with diabetes meds like insulin or metformin. Learn how it affects your liver, why symptoms are hard to spot, and what steps to take if you choose to drink.
