Pharmacogenomics: How Your Genes Affect Your Medications
When you take a pill, your body doesn’t treat it the same way everyone else does. That’s because of pharmacogenomics, the study of how your genes influence how your body processes drugs. Also known as personalized medicine, it’s why one person can take a standard dose of antidepressant and feel better, while another gets dizzy, nauseous, or worse—same drug, same dose, completely different results. This isn’t guesswork. It’s science backed by real data from hospitals and labs.
Your genes control enzymes that break down medications—like CYP2D6 or CYP2C19. These enzymes are like factory workers in your liver. Some people have super-fast workers, others have slow ones. If you’re a fast metabolizer, your body clears drugs too quickly, so the medicine doesn’t work. If you’re slow, the drug builds up and can cause toxic side effects. That’s why warfarin doses vary wildly between people, why some get severe reactions to codeine, and why certain ADHD meds work for one teen but make another feel anxious. This isn’t about lifestyle or compliance—it’s about your DNA.
Pharmacogenomics also explains why some people can’t take statins without muscle pain, or why certain cancer drugs only work for patients with specific gene mutations. It’s not just about picking the right drug—it’s about picking the right dose for your body. Companies now offer genetic tests that tell you how you’ll respond to over 100 common meds, from blood thinners to painkillers. Doctors are starting to use this info before prescribing, especially for high-risk drugs like clozapine, carbamazepine, and abacavir. The goal? Fewer hospital visits, fewer side effects, and better outcomes.
But here’s the catch: most people still don’t know their pharmacogenomic profile. Even if your doctor knows about it, they might not test you unless you’re on a high-risk medication. That’s changing fast. More insurance plans are covering these tests. More labs are making them cheaper. And more research—like the studies showing how genetic testing cuts adverse drug reactions by up to 30%—is pushing it into the mainstream.
What you’ll find below isn’t just theory. These are real stories, real risks, and real solutions from people who’ve been there. From how garlic supplements mess with blood thinners because of your genes, to why metronidazole causes nerve damage in some but not others, to why your ADHD meds might be making you jittery because of caffeine and your CYP1A2 enzyme. This collection pulls from the latest guidelines, patient reports, and clinical data to show you exactly how your biology shapes your treatment—and what to do about it.
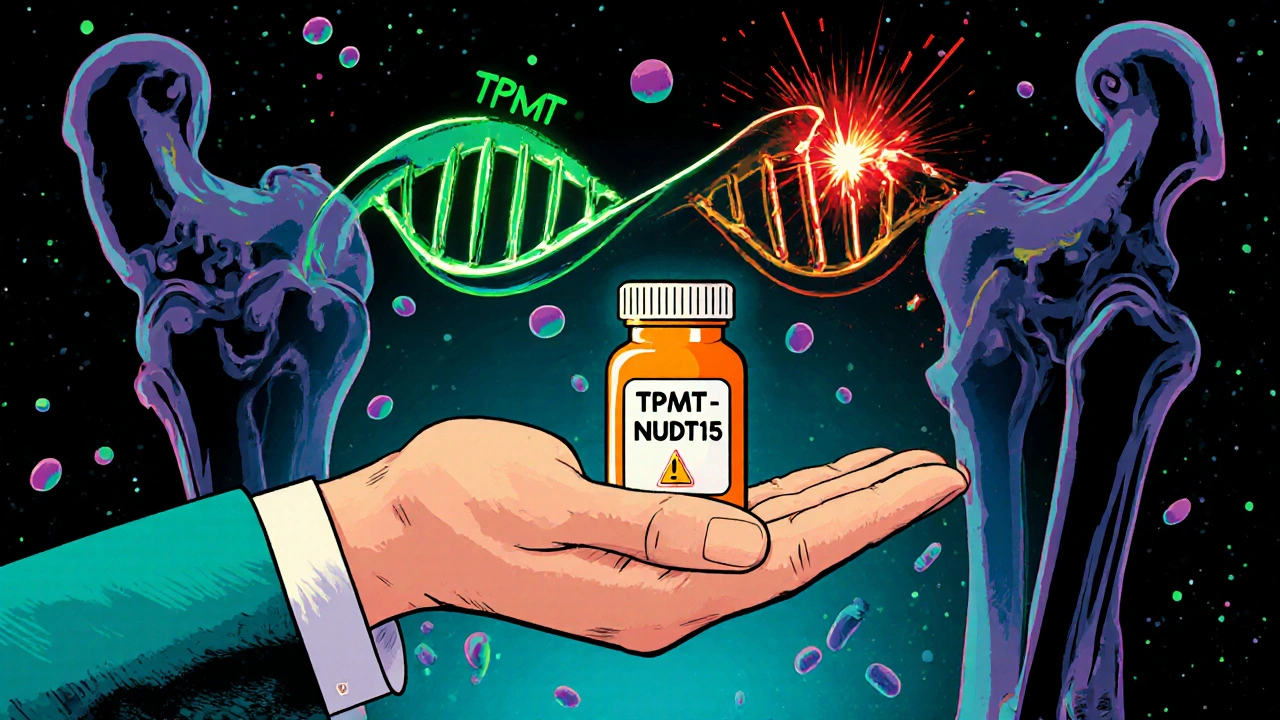
Azathioprine and TPMT Testing: How Genetic Screening Prevents Life-Threatening Side Effects
Azathioprine is an affordable immunosuppressant, but up to 1 in 300 people have a genetic flaw that makes it dangerous. TPMT and NUDT15 testing can prevent life-threatening blood cell loss before it starts.
