Type 2 Diabetes: Symptoms, Causes, and How to Manage It
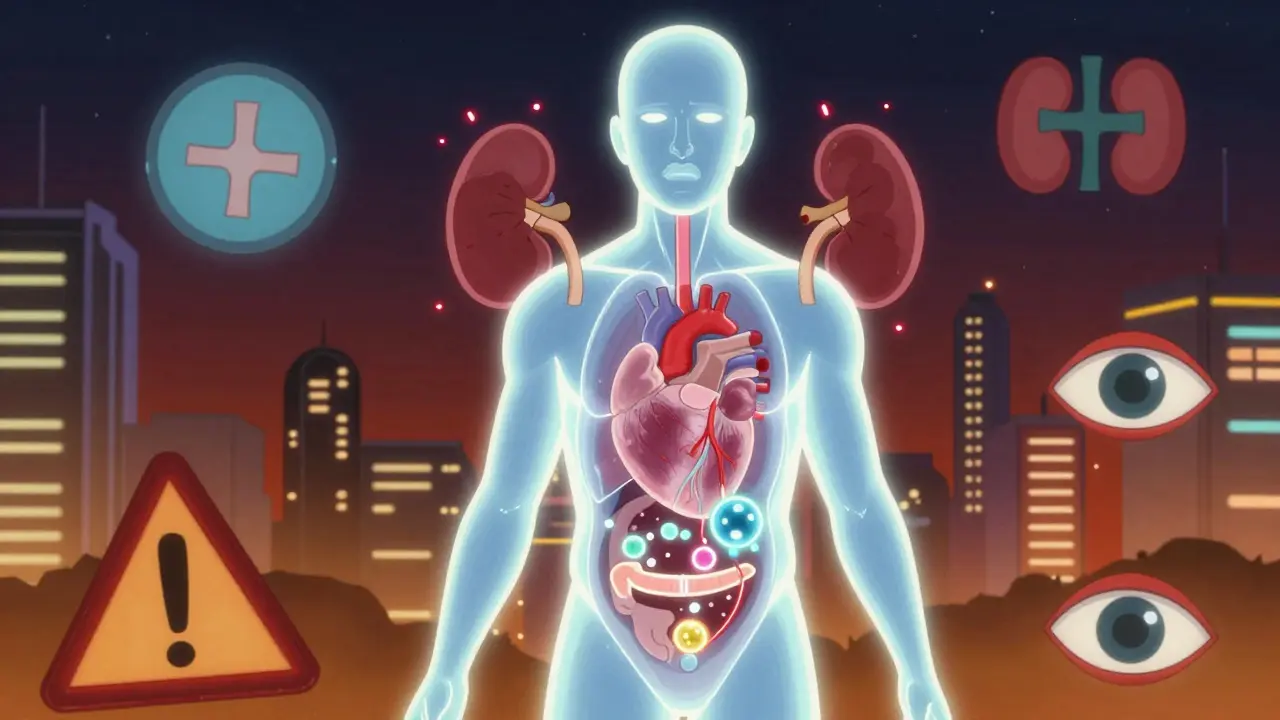
More than 37 million Americans have type 2 diabetes-and nearly 1 in 4 don’t even know it. That’s because the symptoms creep in slowly, often dismissed as just getting older, stressed, or out of shape. But if left unchecked, high blood sugar doesn’t just cause fatigue or frequent bathroom trips. It silently damages your heart, kidneys, nerves, and eyes. The good news? Type 2 diabetes isn’t a death sentence. With the right approach, you can control it, reverse some damage, and live well for decades.
What Exactly Is Type 2 Diabetes?
Type 2 diabetes happens when your body stops responding properly to insulin, the hormone that moves sugar from your blood into your cells for energy. At first, your pancreas tries to compensate by making more insulin. But over time, it gets worn out and can’t keep up. Blood sugar rises, and without intervention, it keeps climbing.
This isn’t just about eating too much sugar. It’s a complex mix of genetics, lifestyle, and biology. Unlike type 1 diabetes-where the immune system destroys insulin-producing cells-type 2 is largely preventable and manageable. It used to be called adult-onset diabetes, but now it’s common in teens and young adults, especially those with obesity or a family history.
Early Signs You Might Be Developing Type 2 Diabetes
The symptoms don’t hit like a lightning strike. They whisper. You might not notice them until something serious happens-a foot ulcer, a heart attack, or a routine blood test that shows your HbA1c is above 6.5%.
- Constant thirst and frequent urination: High blood sugar pulls fluid from your tissues, making you thirsty. Your kidneys work overtime to filter out the extra sugar, leading to more trips to the bathroom-sometimes every hour.
- Unexplained weight loss: Even if you’re eating normally, your body can’t use sugar for fuel, so it starts breaking down muscle and fat instead.
- Extreme fatigue: Your cells are starved for energy. You feel drained even after a full night’s sleep.
- Blurred vision: Sugar pulls fluid from the lenses of your eyes, making it hard to focus.
- Slow-healing cuts or infections: High glucose impairs circulation and weakens your immune system. A small cut can turn into a serious infection.
- Tingling or numbness in hands or feet: This is nerve damage from prolonged high blood sugar. It’s called diabetic neuropathy and affects nearly 70% of people after 10 years.
- Dark, velvety patches on skin: Called acanthosis nigricans, this usually shows up on the neck, armpits, or groin. It’s a visible red flag for insulin resistance.
Here’s the hard truth: 1 in 5 people with type 2 diabetes have no symptoms at all. That’s why regular checkups matter-especially if you’re over 45, overweight, or have a parent or sibling with the condition.
Why Did This Happen to Me? The Real Causes
It’s not your fault. But it’s not random, either. Type 2 diabetes is the result of a perfect storm.
Insulin resistance is the root problem. Your muscle, fat, and liver cells stop listening to insulin. Your pancreas responds by pumping out more insulin-sometimes two or three times the normal amount. Eventually, it burns out.
Obesity is the biggest trigger. People with a BMI over 30 are 80 times more likely to develop type 2 diabetes than those with a BMI under 22. Fat tissue, especially around the abdomen, releases chemicals that interfere with insulin signaling.
Genetics play a big role. If one parent has type 2 diabetes, your risk jumps by 40%. If both have it? You’re looking at nearly a 70% chance. Over 400 genetic variants have been linked to increased risk, and some ethnic groups face much higher rates: Native Americans (14.5%), African Americans (12.1%), Hispanic Americans (11.8%), and Asian Americans (9.5%) compared to non-Hispanic whites (7.4%).
Lack of movement is another major factor. Physical inactivity contributes to nearly 3 in 10 cases worldwide. Sitting all day makes your cells less sensitive to insulin-even if you’re not overweight.
Aging naturally reduces insulin sensitivity. But the scary trend? More than 287,000 Americans under 20 now have type 2 diabetes. That’s not just a health issue-it’s a societal one.
What Happens If You Don’t Manage It?
Uncontrolled type 2 diabetes doesn’t just cause discomfort. It quietly destroys your body.
- Heart disease: Two to four times higher risk of heart attack or stroke. About 70% of deaths in people with diabetes are linked to cardiovascular problems.
- Kidney failure: Diabetes causes 44% of new cases of kidney failure in the U.S. That means dialysis or transplant for many.
- Nerve damage: Diabetic neuropathy leads to foot ulcers in 15-20% of patients. Of those, up to a quarter end up needing amputation.
- Blindness: Diabetic retinopathy affects nearly 30% of adults with diabetes. It’s the leading cause of new blindness in working-age adults.
- Dementia: People with diabetes have a 2-3 times higher risk of Alzheimer’s. Some researchers even call it “type 3 diabetes” because of how insulin resistance affects the brain.
- Depression: One in four people with diabetes also has depression. And that doubles the risk of early death.
These aren’t distant threats. They’re real, measurable outcomes-and they’re preventable.
How to Manage Type 2 Diabetes-The Proven Way
There’s no magic pill. But there is a proven path: lifestyle changes, smart medications, and consistent monitoring.
1. Diet That Works
You don’t need to go keto or starve yourself. Focus on real food: vegetables, lean proteins, whole grains, nuts, and healthy fats. Cut out sugary drinks, processed snacks, and refined carbs like white bread and pastries.
The National Diabetes Prevention Program showed that losing just 7% of your body weight (like 15 pounds if you weigh 200) cuts your risk of developing diabetes by 58%. That’s more effective than any drug.
Try the plate method: half your plate non-starchy veggies (broccoli, spinach, peppers), one-quarter lean protein (chicken, fish, tofu), one-quarter whole grains or starchy veggies (quinoa, sweet potato). Eat slowly. Stop when you’re full.
2. Move Your Body
Exercise isn’t optional-it’s medicine. Aim for 150 minutes a week of moderate activity: brisk walking, swimming, cycling. Even 10-minute walks after meals help lower blood sugar spikes.
Strength training twice a week builds muscle, which improves insulin sensitivity. You don’t need a gym. Bodyweight squats, push-ups, and resistance bands work just fine.
3. Medications When Needed
Metformin is still the first-line drug. It lowers blood sugar, helps with weight loss, and is safe for most people. It reduces HbA1c by 1-2%.
Newer drugs like GLP-1 agonists (semaglutide, liraglutide) and SGLT2 inhibitors (empagliflozin, dapagliflozin) do more than lower sugar-they protect your heart and kidneys. Some help you lose 5-15 pounds.
In 2022, the FDA approved tirzepatide (Mounjaro), a dual-action drug that reduced HbA1c by over 2% and led to 11-15 pounds of weight loss in trials. It’s now being used for type 2 diabetes, not just weight loss.
4. Monitor Your Blood Sugar
Testing isn’t just for insulin users. Even if you’re on pills or just diet and exercise, checking your levels helps you see what works. A continuous glucose monitor (CGM) can show you how your body reacts to meals, sleep, and stress.
CGM use among Medicare beneficiaries jumped from 1.2% in 2017 to 12.7% in 2022. More coverage means more people are catching problems early.
5. Sleep and Stress Matter Too
Chronic stress raises cortisol, which raises blood sugar. Poor sleep messes with insulin sensitivity. Aim for 7-8 hours of quality sleep. Practice breathing exercises, walking, or meditation. These aren’t luxuries-they’re part of your treatment plan.

Can Type 2 Diabetes Be Reversed?
Yes. Not cured. But reversed-meaning you no longer need medication to keep your blood sugar in a healthy range.
The DIALECT trial showed that 46% of people with type 2 diabetes for less than six years achieved remission after a year of a very low-calorie diet (825-853 calories/day) followed by gradual food reintroduction. Their HbA1c dropped below 6.5% without drugs.
This isn’t about extreme diets forever. It’s about resetting your metabolism. Lose weight, get active, and give your pancreas a break. Many people stay in remission for years-if they stick with healthy habits.
What’s Next? The Future of Type 2 Diabetes Care
The tools are getting better. Hybrid closed-loop systems (like the MiniMed 780G) now help people with type 2 diabetes maintain blood sugar in the target range 71% of the time-up from 51% with traditional methods.
Researchers are using AI to predict who’s at risk before they even develop symptoms. The NIH’s All of Us program is collecting data from 1 million people to understand why diabetes hits some groups harder than others.
But technology won’t fix what society breaks. The real challenge? Access. Healthy food, safe places to walk, affordable medications, and mental health support aren’t equally available to everyone.
Diabetes costs the U.S. $413 billion a year. But investing in prevention saves money-$5,700 per person over 10 years, according to the CDC.
Where Do You Start Today?
Don’t wait for symptoms to get worse. Don’t wait for a crisis.
- Get your HbA1c checked if you haven’t had it in the last year.
- Walk for 15 minutes after dinner.
- Swap soda for sparkling water.
- Write down what you eat for three days. Look for patterns.
- Talk to your doctor about metformin if you’re prediabetic.
Type 2 diabetes is a challenge-but it’s not your identity. It’s a signal. A chance to take back control. The science is clear: small, consistent changes today prevent big problems tomorrow.
Can type 2 diabetes be cured?
There’s no permanent cure, but many people achieve remission-meaning their blood sugar stays normal without medication. This usually happens after significant weight loss and sustained lifestyle changes. The key is maintaining those habits long-term.
Is metformin safe for long-term use?
Yes. Metformin has been used safely for over 60 years. Common side effects like stomach upset usually fade after a few weeks. Rarely, it can affect vitamin B12 levels, so your doctor may check that annually. It doesn’t cause low blood sugar on its own and may even help with weight loss.
Do I need to test my blood sugar every day?
Not necessarily. If you’re on insulin or have trouble controlling your levels, daily testing helps. If you’re managing with diet and metformin, checking a few times a week-or using a CGM-can give you enough insight. Talk to your doctor about what’s right for your situation.
Can I still eat carbs with type 2 diabetes?
Absolutely. But the type and amount matter. Choose whole grains, legumes, fruits, and starchy vegetables over white bread, pasta, and sugary cereals. Pair carbs with protein or fat to slow absorption. Portion control is key-most people do better with 30-45 grams of carbs per meal.
What’s the best exercise for type 2 diabetes?
The best exercise is the one you’ll stick with. Walking is ideal for most people-it’s low-impact and effective. Combine it with strength training (even light weights or resistance bands) twice a week. Muscle burns more glucose, so building it improves insulin sensitivity.
How do I know if my diabetes is getting worse?
Watch for rising HbA1c levels, increased thirst or urination, unexplained weight loss, frequent infections, or numbness/tingling in your hands or feet. If your current plan isn’t keeping your blood sugar in range, it’s time to revisit your treatment with your doctor. Progress isn’t always linear-adjustments are normal.
Can stress cause type 2 diabetes?
Stress doesn’t directly cause it, but it makes it harder to manage. Chronic stress raises cortisol, which increases blood sugar. It can also lead to poor sleep, emotional eating, and skipping exercise-all of which worsen insulin resistance. Managing stress isn’t optional-it’s part of treatment.
Is type 2 diabetes hereditary?
Yes. If one parent has type 2 diabetes, your risk is about 40%. If both have it, your risk jumps to nearly 70%. But genetics aren’t destiny. Even with a strong family history, losing weight and staying active can delay or prevent the disease.

ellen adamina
January 14, 2026 AT 14:59Gloria Montero Puertas
January 16, 2026 AT 12:23Tom Doan
January 18, 2026 AT 00:23Dan Mack
January 18, 2026 AT 23:49Amy Vickberg
January 19, 2026 AT 07:42Nicholas Urmaza
January 21, 2026 AT 01:11Sarah Mailloux
January 22, 2026 AT 00:15Nilesh Khedekar
January 22, 2026 AT 06:57Jami Reynolds
January 22, 2026 AT 21:15Amy Ehinger
January 24, 2026 AT 01:53RUTH DE OLIVEIRA ALVES
January 25, 2026 AT 16:27