Diabetes — Symptoms, Tests & Daily Management
Diabetes changes how your body handles sugar. Whether you’re newly diagnosed or trying to stay on top of it, small, consistent steps make the biggest difference. This page gives clear, practical actions you can use today to check symptoms, read test results, and control daily blood sugar without the fluff.
Quick signs and tests
Common signs include increased thirst, peeing more than usual, unexplained tiredness, slow-healing cuts, and blurred vision. If you notice these, get a simple A1C or fasting glucose test. A1C shows average blood sugar over 2–3 months; many adults aim for under 7%, but your target may differ based on age and health.
Home glucose meters let you see moment-to-moment changes. Typical targets many clinicians use are: fasting about 80–130 mg/dL and under 180 mg/dL two hours after a meal. Treat numbers as clues — patterns matter more than a single reading.
Daily habits that move the needle
Move your body. Aim for about 150 minutes of moderate activity a week — walking counts. Exercise lowers blood sugar and improves how meds work. You don’t need intense workouts; 30 minutes most days is a great start.
Watch portion sizes and carbs. Instead of strict diets, pick consistent, simple swaps: whole grains over white bread, fruit instead of sugary drinks, and protein at meals to slow sugar spikes. If you count carbs, keep it steady across meals so meds and insulin work predictably.
Know your meds. Metformin is often the first pill for type 2. Other options include newer classes like SGLT2 and GLP-1 drugs, which can help weight and heart health. People with type 1 need insulin. Always follow your prescriber’s plan and ask about side effects and how a new drug fits your goals.
Prevent complications with basic checks: brush and floss daily, inspect feet for cuts or sores, and get regular eye and kidney screenings. High blood pressure and cholesterol also matter; treating them lowers risk of heart and kidney problems.
Handle lows and highs simply. For low blood sugar (sweaty, shaky, confused), eat 15 grams of fast carbs — 4 glucose tablets or 4 oz juice — then recheck in 15 minutes. For very high sugar with nausea, deep breathing trouble, or fruity breath, seek urgent care; severe highs can be an emergency.
Stress, sleep, and routine matter. Poor sleep or high stress raises blood sugar. Small routines — same meal times, regular sleep, and a consistent activity plan — make glucose more predictable and your life easier.
Talk with your care team. Bring a log of readings and questions to appointments. If costs or access are an issue, ask about generic meds, support programs, or simple self-care steps you can start right away. You don’t have to manage diabetes alone — practical tools and steady habits help you stay in control.
How progesterone can help with insulin resistance and diabetes
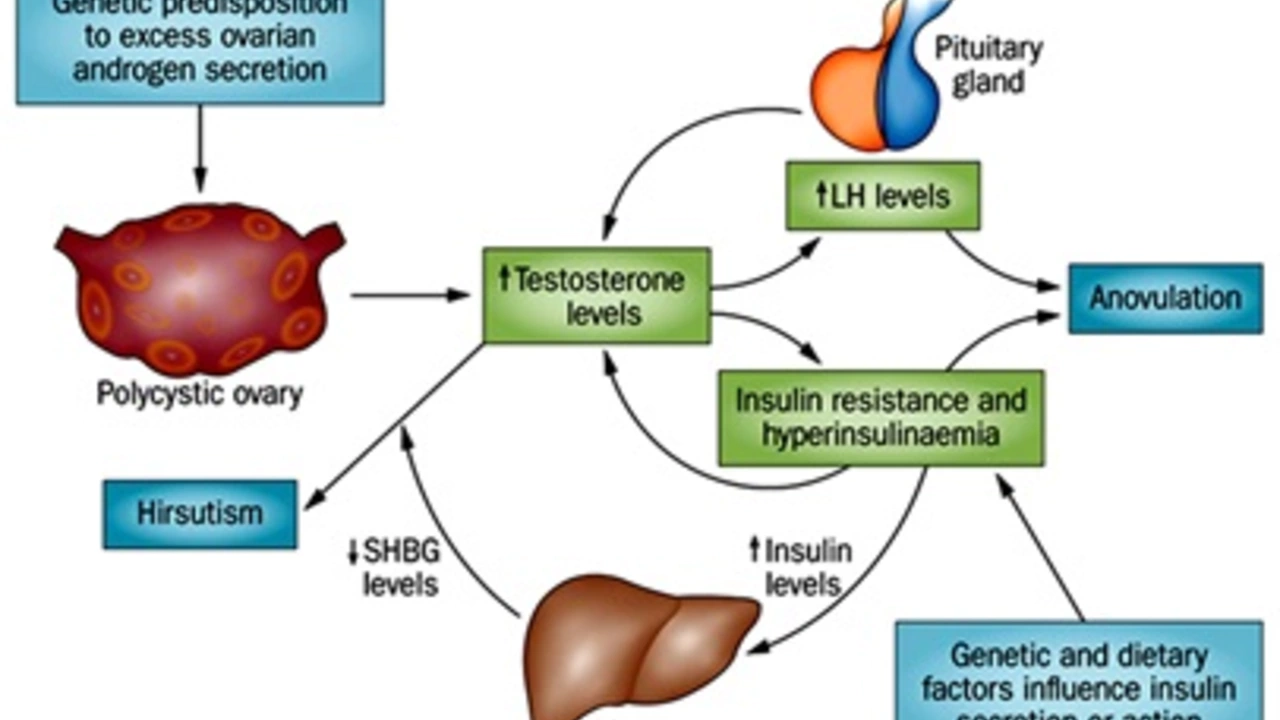
In my recent exploration of health topics, I've discovered some fascinating insights on how progesterone can aid in combating insulin resistance and diabetes. It appears that progesterone, a hormone naturally produced in the body, improves insulin sensitivity and helps in regulating blood sugar levels. Research suggests that it may also play a protective role against the onset of type 2 diabetes. However, the relationship between hormones and insulin resistance is complex and more research is needed. It's an intriguing area of study which could potentially offer new approaches in managing diabetes.
