Hormone Therapy
Feeling tired, losing sex drive, getting hot flashes, or noticing unexplained weight changes? Those can be signs of hormone imbalance. Hormone therapy replaces or adjusts hormones your body no longer makes correctly. It can bring big benefits, but it also carries risks. This page gives clear, practical info so you can talk with your doctor and make better choices.
Who might need hormone therapy
People get hormone therapy for different reasons. Menopause symptoms like hot flashes, night sweats, mood swings, and vaginal dryness are commonly treated with estrogen or estrogen plus progesterone. Men with low testosterone may try testosterone replacement for low energy, low libido, or muscle loss. Thyroid hormone treats hypothyroidism, and insulin is essential for type 1 diabetes. Less common uses include growth hormone for deficiency and corticosteroids for adrenal problems.
Not everyone with symptoms needs treatment. Doctors look at symptoms, blood tests, medical history, and personal risks before recommending therapy. Age, heart disease, blood clot risk, and cancer history matter when choosing the right option.
What to expect and how to stay safe
Before starting, expect baseline tests: hormone levels, blood count, liver function, lipids, and other checks based on your health. Start at the lowest effective dose and recheck levels and symptoms after a few months. Regular follow-ups help catch side effects early and let your doctor adjust the plan.
Common side effects vary by treatment. Estrogen can cause breast tenderness, bloating, or spotting and slightly raise blood clot risk. Testosterone can change mood, raise red blood cell count, or affect cholesterol. Thyroid overdosing causes anxiety and fast heartbeat; underdosing leaves symptoms unchanged. Report new chest pain, shortness of breath, sudden swelling, severe headaches, or vision changes right away.
Ask these practical questions: What are the likely benefits and how soon will I notice them? What tests will you run before and during treatment? How long should I expect to stay on therapy? What are the alternatives or lifestyle steps I can try first? How will this interact with my other medicines?
Choose the right form for your life. Patches, gels, pills, injections, and implants each have pros and cons. Patches avoid first-pass liver effects; pills are easy but may affect liver function; gels give steady dosing but require careful handling. Your doctor should explain which form fits your needs and routine.
Small lifestyle changes make a big difference. Sleep, balanced diet, resistance exercise, and quitting smoking often improve symptoms and reduce risks. If you're unsure where to start, ask your provider for a stepwise plan combining lifestyle and medical options.
Hormone therapy can work well when it's tailored to you and monitored regularly. Keep records of symptoms and side effects, bring questions to appointments, and get a second opinion if something feels off. For reliable drug info and more practical guides, check resources on Top-Meds.org.
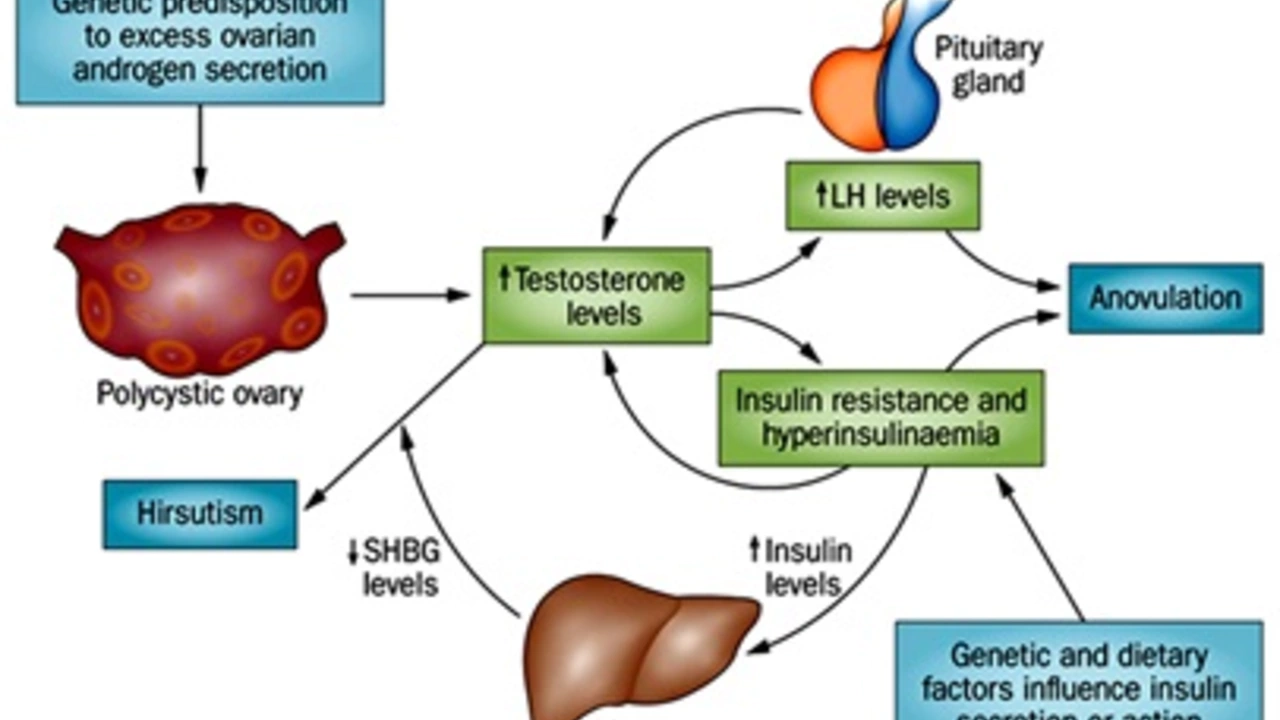
How progesterone can help with insulin resistance and diabetes
In my recent exploration of health topics, I've discovered some fascinating insights on how progesterone can aid in combating insulin resistance and diabetes. It appears that progesterone, a hormone naturally produced in the body, improves insulin sensitivity and helps in regulating blood sugar levels. Research suggests that it may also play a protective role against the onset of type 2 diabetes. However, the relationship between hormones and insulin resistance is complex and more research is needed. It's an intriguing area of study which could potentially offer new approaches in managing diabetes.
