OIH: Understanding Off-Label Use, Interactions, and Health Risks in Medications
When you hear OIH, Off-Label Use and Health risks in pharmaceutical practice. Also known as Off-Label Indication and Health risks, it refers to the use of a drug for purposes not officially approved by the FDA—yet commonly practiced in clinics, hospitals, and even at home. This isn’t rare. Up to 20% of all prescriptions in the U.S. are for off-label uses, especially in psychiatry, oncology, and pediatrics. But just because a doctor prescribes it doesn’t mean it’s safe—or that you’re being told the full story.
One major risk tied to OIH is drug interactions, when two or more medications affect each other’s effectiveness or safety. Think garlic supplements thinning your blood while you’re on warfarin, or caffeine boosting Adderall to dangerous heart-stress levels. These aren’t theoretical—they’re documented in real cases that led to ER visits and hospitalizations. Then there’s adverse effects, unintended, harmful reactions to medications. Metronidazole causing nerve damage after just a few weeks. Azathioprine triggering life-threatening blood cell loss in people with undetected TPMT gene flaws. These aren’t side effects you can ignore—they’re red flags that need testing, monitoring, and open communication with your provider.
OIH isn’t just about what’s written on the bottle. It’s about what’s hidden: the unapproved uses, the unlabeled risks, the ignored lab tests. It’s why pharmacists now use barcode systems and AI to catch errors before they reach you. Why some pharmacies require prior authorization for certain generics—not because they’re expensive, but because they’re risky if used incorrectly. Why switching pharmacies matters more than you think, especially with controlled substances or complex regimens. And why knowing where to find real side effect data—like DailyMed or VigiAccess—isn’t optional, it’s essential.
You’re not just taking a pill. You’re managing a system. And when that system ignores OIH, people get hurt. The posts below break down exactly how these hidden risks play out in real life—from chemotherapy safety protocols to how alcohol crashes blood sugar in diabetics, from counterfeit drug traps to why your kidney diet needs phosphorus limits. This isn’t theory. It’s what’s happening right now in pharmacies, clinics, and homes across the country. What you read here could keep you—or someone you love—out of the hospital.
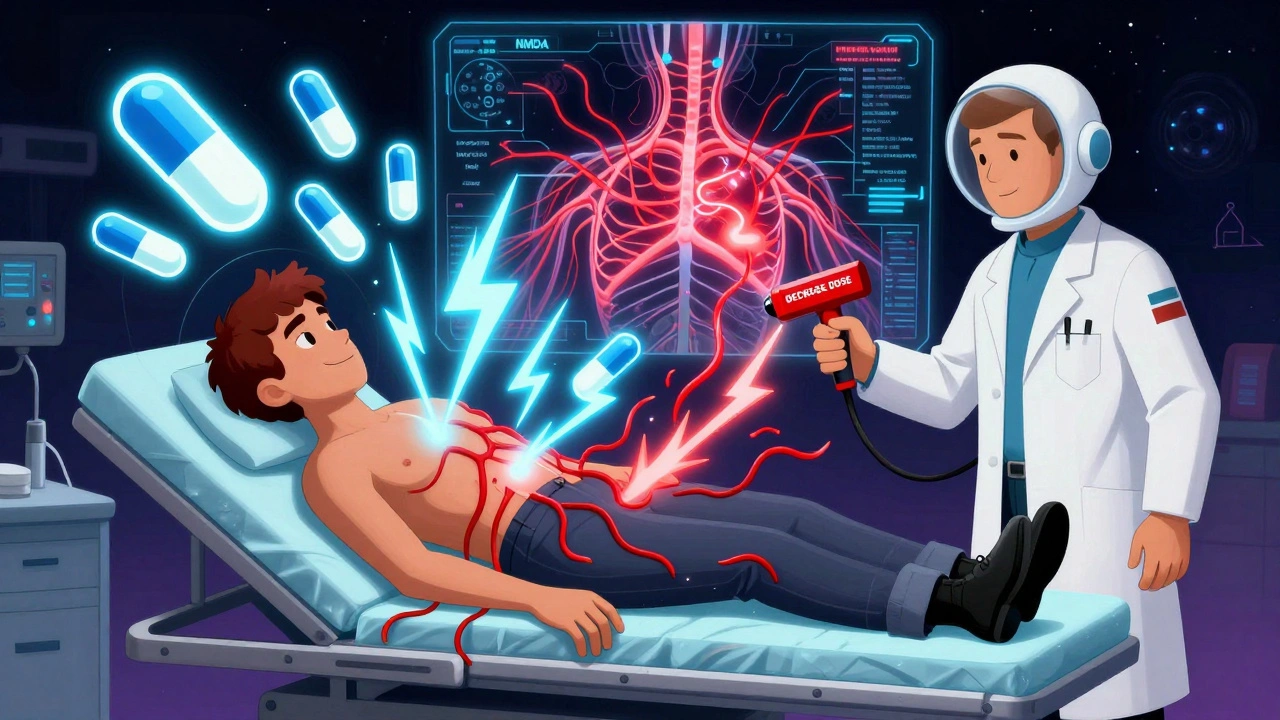
Opioid-Induced Hyperalgesia: How to Spot and Treat It
Opioid-induced hyperalgesia (OIH) is when long-term opioid use makes pain worse instead of better. Learn how to recognize the signs, why it happens, and what treatments actually work - from tapering doses to ketamine and genetic testing.
