Opioid Pain Treatment: Safe Use, Risks, and Alternatives
When it comes to opioid pain treatment, a class of powerful drugs used to manage moderate to severe pain. Also known as narcotic analgesics, they include medications like oxycodone, hydrocodone, and morphine—effective for acute injuries or cancer pain, but risky when used long-term. Many people start with a prescription after surgery or injury, but without careful monitoring, these drugs can lead to dependence, tolerance, or worse.
One major concern is opioid addiction, a chronic condition where the brain becomes reliant on the drug to feel normal. This isn’t about willpower—it’s biology. The brain’s reward system changes, making cravings intense and withdrawal painful. That’s why medication-assisted treatment, using FDA-approved drugs like methadone, buprenorphine, or naltrexone to stabilize brain chemistry is now the gold standard for recovery. It doesn’t replace one drug with another—it restores balance.
Another critical tool is naloxone, a life-saving medication that reverses opioid overdoses in minutes. It’s not just for addicts—it’s for anyone who takes opioids, even as prescribed. Keeping naloxone on hand, whether at home or in a workplace, can mean the difference between life and death. Many pharmacies now offer it without a prescription, and training is often free through local health departments.
Long-term opioid use also brings side effects: constipation, sleep issues, hormonal changes, and even increased pain sensitivity over time—a condition called opioid-induced hyperalgesia. That’s why doctors now recommend trying non-opioid options first: physical therapy, NSAIDs like ibuprofen, nerve blocks, or even cognitive behavioral therapy. For chronic pain, a multidisciplinary approach works better than pills alone.
And if you’re switching pharmacies or refilling prescriptions, know this: federal rules now limit how often you can get refills on controlled substances. Some states require electronic prescriptions only. If you’ve been on opioids for more than a few weeks, your doctor should be checking in regularly—not just for refills, but for signs of misuse or declining function.
Below you’ll find real, practical advice from people who’ve been through this—whether they’re managing pain after an accident, helping a loved one recover from addiction, or navigating insurance hurdles to get safer alternatives. These aren’t theory pieces. They’re guides written by pharmacists, clinicians, and patients who’ve seen what works—and what doesn’t.
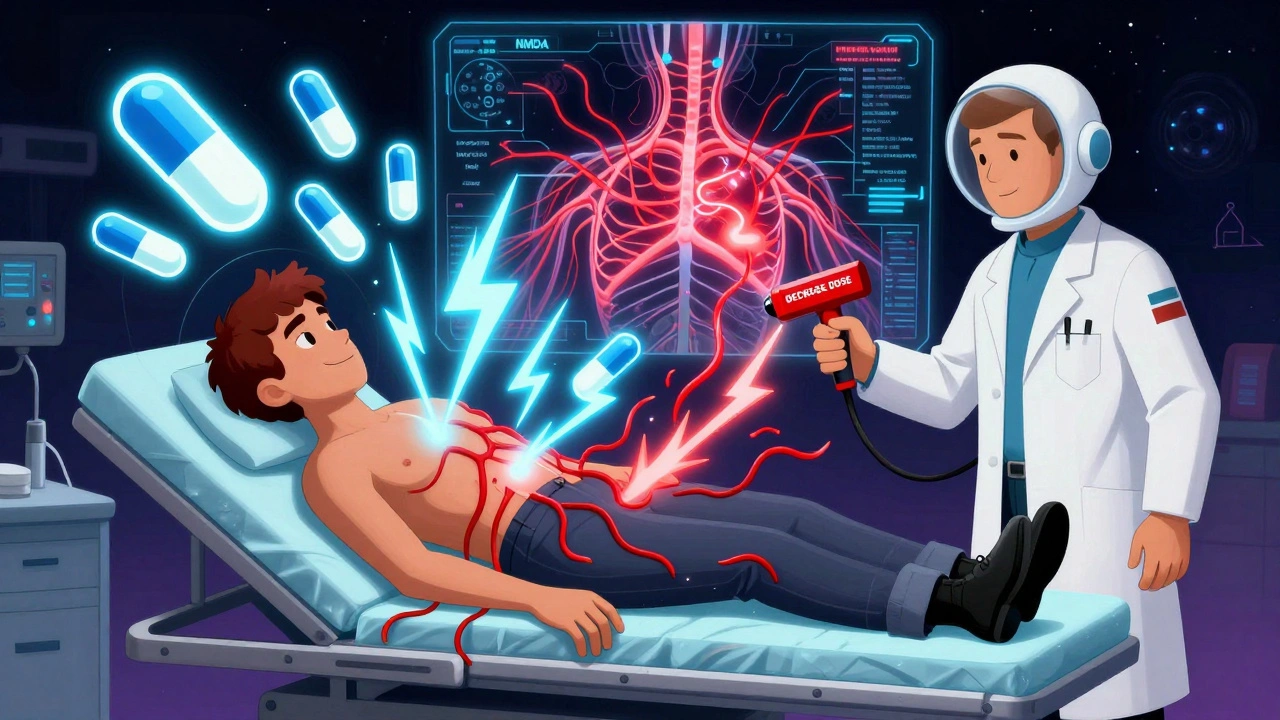
Opioid-Induced Hyperalgesia: How to Spot and Treat It
Opioid-induced hyperalgesia (OIH) is when long-term opioid use makes pain worse instead of better. Learn how to recognize the signs, why it happens, and what treatments actually work - from tapering doses to ketamine and genetic testing.
