Opioid Side Effects: What You Need to Know Before Taking These Medications
When you take opioids, a class of powerful pain-relieving drugs that include prescription pills like oxycodone and hydrocodone, as well as illegal drugs like heroin. Also known as narcotics, these medications work by binding to special receptors in your brain and spinal cord to block pain signals. But they also affect areas that control breathing, mood, and reward—making them highly effective for pain and dangerously easy to misuse. The most common opioid side effects include drowsiness, nausea, constipation, and dizziness. These aren’t just inconveniences—they can be signs that your body is struggling with the drug’s impact. For many, constipation becomes so severe it leads to bowel obstruction. Drowsiness can turn into dangerous respiratory depression, especially when mixed with alcohol or sleep aids.
Long-term use brings even bigger risks. Your body adapts, needing more of the drug just to feel normal—that’s tolerance. Then comes dependence, where stopping the drug triggers opioid withdrawal, a painful set of symptoms including muscle aches, insomnia, vomiting, and intense anxiety. And for some, dependence turns into addiction, where the drive to use overrides health, relationships, and safety. naloxone, a fast-acting medication that can reverse an opioid overdose in minutes, is now carried by first responders, pharmacies, and even friends of people using opioids. It’s not a cure, but it’s the best shot at survival when breathing stops.
What most people don’t realize is that opioid side effects don’t just happen to users—they affect families, doctors, and communities. A single prescription can start a chain reaction: a back pain patient gets pills, takes them longer than needed, runs out, and turns to cheaper street drugs. That’s why monitoring, education, and alternatives matter. If you’re on opioids, ask your doctor about the lowest effective dose, the shortest possible time, and what to do if you notice changes in your mood, sleep, or breathing. Keep naloxone on hand if you live with someone who uses opioids. And if you’re worried about dependence, help is available through medication-assisted treatment like methadone or buprenorphine—proven tools that reduce cravings and keep people alive.
Below, you’ll find real-world advice from people who’ve dealt with these issues firsthand—from how to spot early signs of overdose to how to safely switch off opioids without crashing. These aren’t theoretical guides. They’re practical, tested strategies from patients, pharmacists, and clinicians who’ve seen what happens when things go wrong—and what works when they don’t.
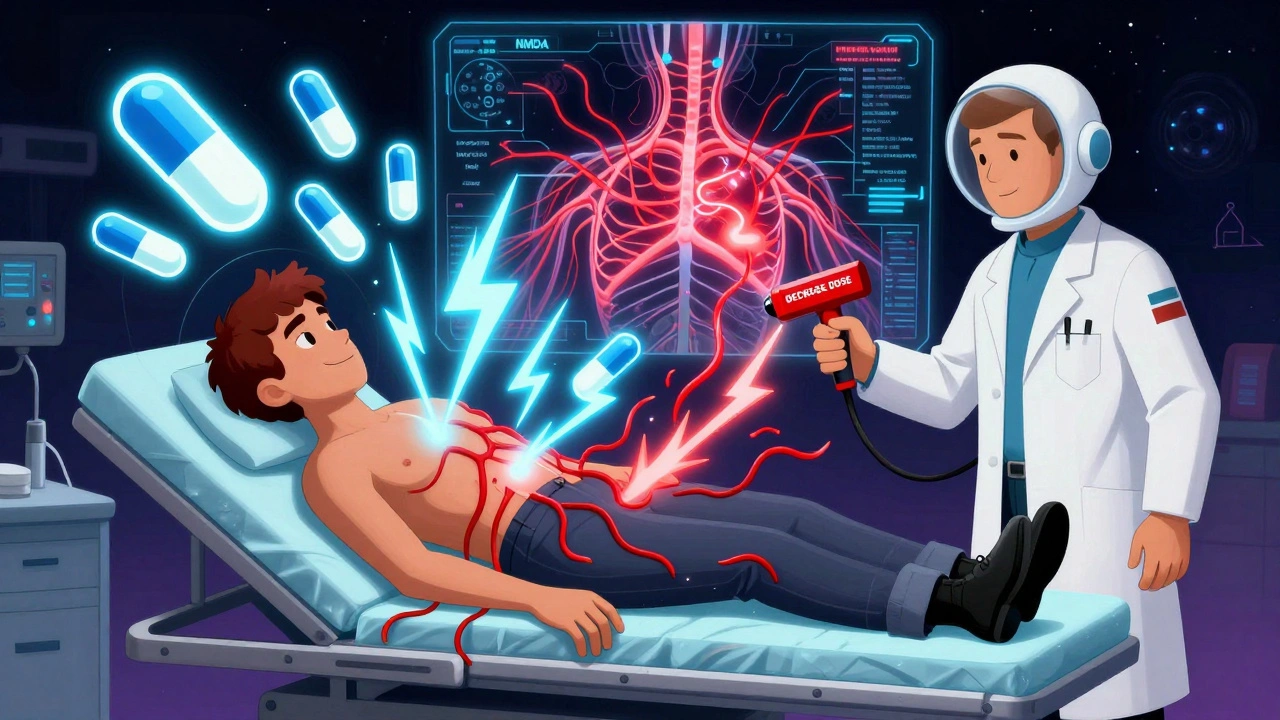
Opioid-Induced Hyperalgesia: How to Spot and Treat It
Opioid-induced hyperalgesia (OIH) is when long-term opioid use makes pain worse instead of better. Learn how to recognize the signs, why it happens, and what treatments actually work - from tapering doses to ketamine and genetic testing.
