SGLT2 Inhibitors: What They Are, How They Work, and What You Need to Know
When you hear SGLT2 inhibitors, a class of prescription drugs used to treat type 2 diabetes by making the kidneys remove sugar through urine. Also known as gliflozins, they work differently than most diabetes meds—instead of forcing your body to use insulin better or making more of it, they let your body flush out extra sugar naturally. That’s why they’re not just for blood sugar control—they’re also used to protect your heart and kidneys in people with diabetes or even those without it.
These drugs include empagliflozin, a brand-name drug that reduced heart failure hospitalizations in large clinical trials, canagliflozin, linked to lower risk of kidney disease progression in people with diabetes, and dapagliflozin, shown to improve survival in heart failure patients, even without diabetes. They’re often prescribed when metformin alone isn’t enough, or when patients need extra heart or kidney protection. Unlike insulin or sulfonylureas, they rarely cause low blood sugar on their own—which makes them safer for many people.
But they’re not without risks. The most common side effect is urinary tract or yeast infections because sugar in urine feeds bacteria and fungi. Dehydration and dizziness can happen too, especially if you’re also on blood pressure meds. And while rare, a serious condition called Fournier’s gangrene—a fast-spreading infection in the genital area—has been reported. That’s why it’s important to know the signs: pain, swelling, fever, or redness in the genital area. If you see any of those, call your doctor right away.
These drugs also interact with other meds. For example, if you’re taking diuretics or blood pressure pills, your doctor will likely start you on a lower dose to avoid drops in blood pressure. And if you’re scheduled for surgery or imaging with contrast dye, you might need to stop them temporarily—your kidneys need a break.
What’s interesting is how these drugs connect to other health issues you might be managing. If you’re on metformin and your kidneys aren’t handling it well, an SGLT2 inhibitor might be a better long-term option. If you’ve got heart failure, these drugs can reduce hospital visits. If you’re struggling with weight loss, many patients lose a few pounds on them—not because they’re appetite suppressants, but because they’re flushing out calories as sugar. And if you’re dealing with chronic kidney disease, they slow decline better than most other diabetes drugs.
There’s also a growing list of people who aren’t diabetic but still benefit. Studies show SGLT2 inhibitors help those with heart failure—even without diabetes—and they’re now being tested in people with obesity, fatty liver disease, and even certain kidney disorders. They’re becoming less of a "diabetes drug" and more of a "protective tool" for multiple organs.
Below, you’ll find real-world advice on how these drugs fit into daily life: what to do if you miss a dose, how they interact with alcohol or supplements, how to spot early signs of trouble, and how to talk to your pharmacist about switching or combining them safely. These aren’t theoretical discussions—they’re based on what patients actually experience and what doctors are seeing in clinics today.
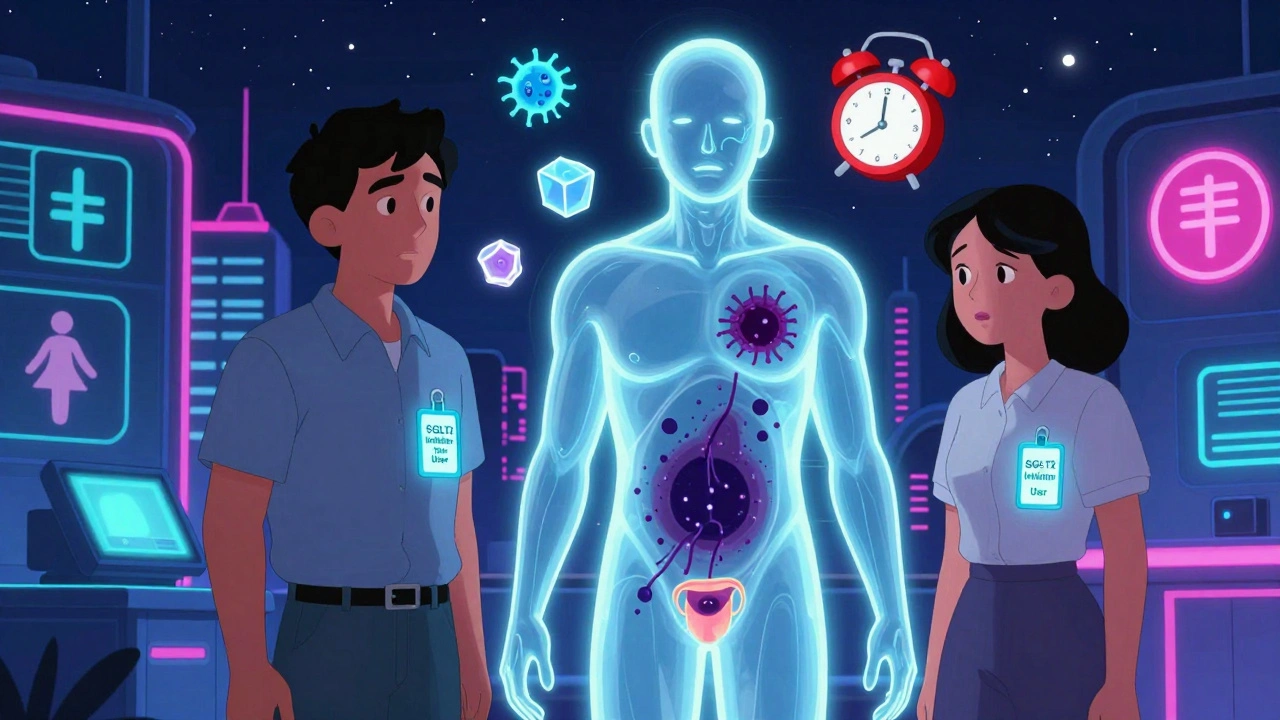
SGLT2 Inhibitors and Fournier’s Gangrene: What You Need to Know Now
SGLT2 inhibitors help manage diabetes and protect the heart and kidneys, but they carry a rare risk of Fournier’s gangrene. Learn the early warning signs and what to do immediately if you notice them.
